Background: High levels of interprofessional collaboration and communication have been shown to lead to better patient safety outcomes, improved patients’ satisfaction and quality of care, as well as higher job satisfaction for doctors and nurses alike. Yet, challenges to nurse-doctor collaborations exist. One way of improving interprofessional collaboration may be through structured co-teaching by nurses and doctors. However, nurse-doctor co-teaching remains an under-explored area of research.
Purpose: We created, designed and implemented a first-of-its-kind Nurse-Doctor Co-Teaching initiative on the General Medicine Service. The goal was to model nurse-doctor collaboration through nurse and doctor design, practice and presentation of interactive teaching sessions to residents and nurses.
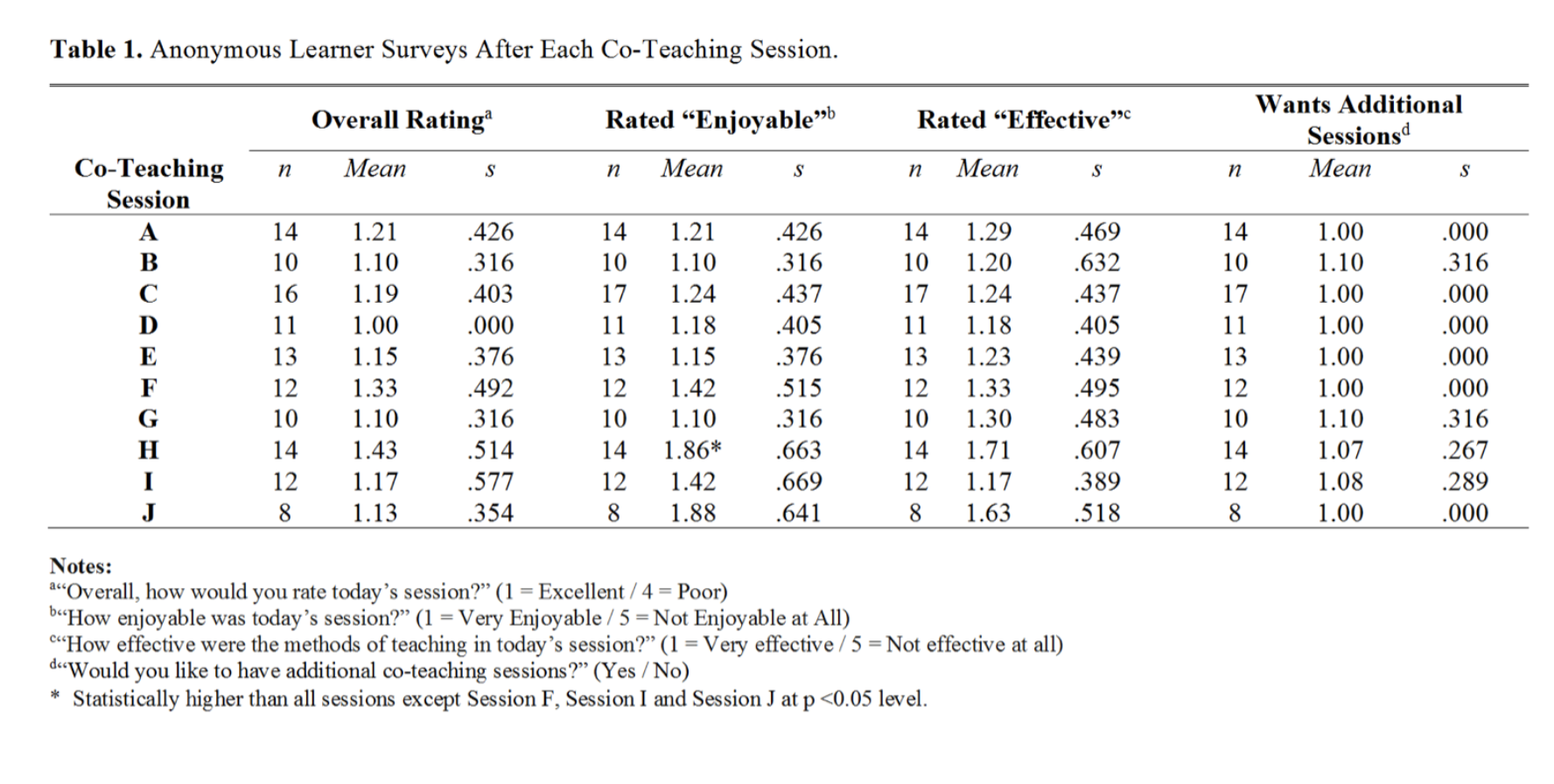
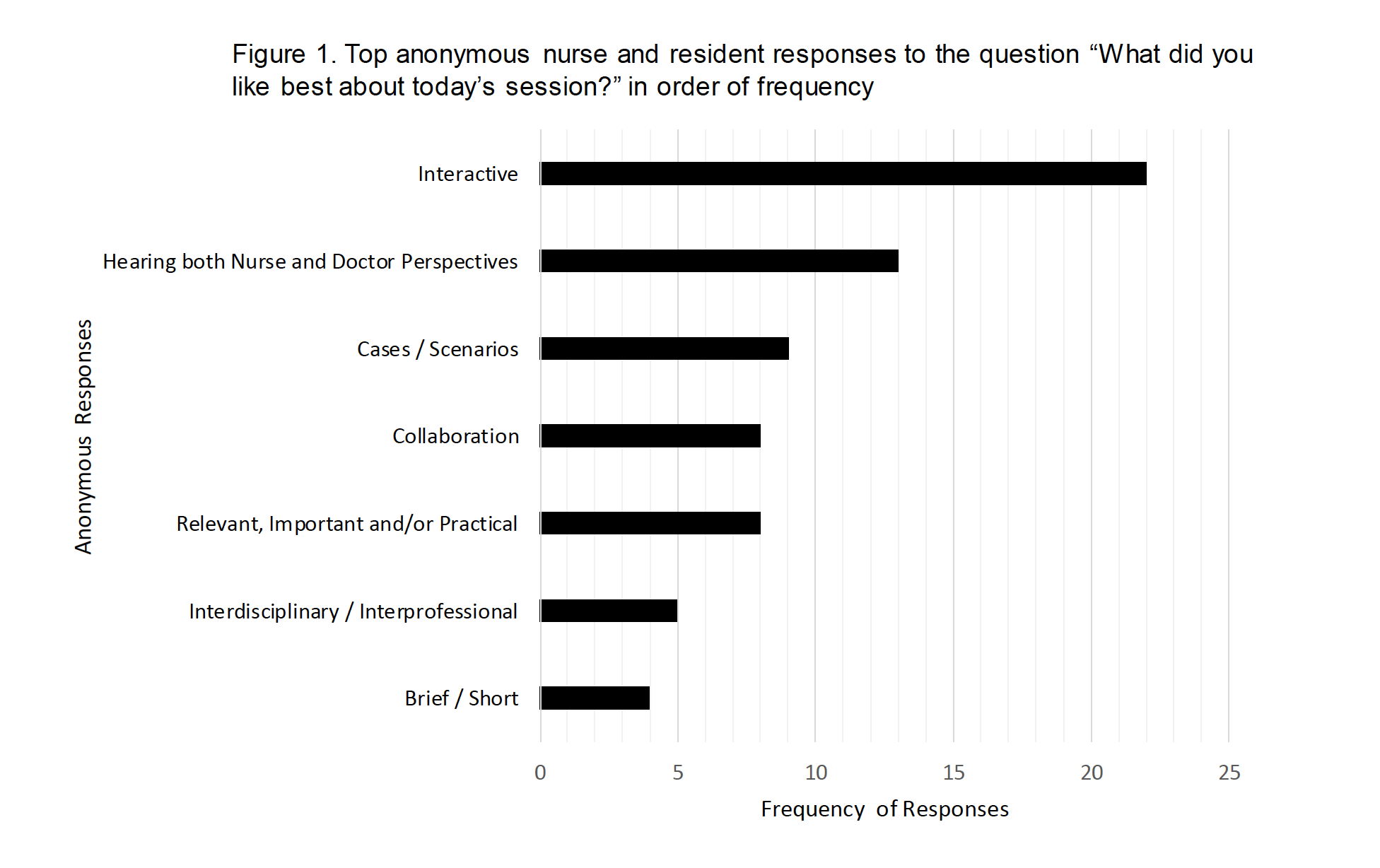
Description: Ten nurses and ten hospitalists volunteered to co-teach as pairs. Each pair decided on a topic and prepared an interactive, 30-minute teaching presentation under the guidance of the project’s educational team. The team encouraged interactive methods to promote active learning. The teaching sessions were presented to a group of residents and nurses weekly in the fall of 2019. Final topics included: Arterial Blood Gases, Alcohol Withdrawal and CIWA, Hyponatremia, Interruptions on the Medical Ward, Opioid Withdrawal and COWS, C. Difficile Testing and Treatment, Telemetry, Catheter Associated Urinary Tract Infections, Testing and Treatment of H. pylori, and Venous Thromboembolism. Sessions were videotaped and placed on the hospital’s Video Library Education website. Both nurse and resident learners completed an IRB approved survey after each session to assess the efficacy of the educational content and interactive methods on a Likert scale ranging from Excellent (1) to 4 (Poor). We collected nine days of Pre-Co-Teaching and Post-Co-Teaching surveys from residents and nurses on the medical floor about their interactions with each other on daily rounds and analyzed these for any significant differences. Nurses’ comfort with asking residents about an order significantly improved in the Post-Teaching period (N=41 Nurses) compared to the Pre-Teaching period (N=41 Nurses) by 14 percentage points going from 85.4% to 100 % (p value=0.01). No other significant differences were noted. Overall ratings for each session are shown in Table 1 and are in the Excellent range between 1.00 to 1.43 on the Likert scale. No significant difference was noted for the overall rating among sessions. Spontaneous resident and nurse responses to the question “What did you like best?” are grouped according to the most frequent responses in Figure 1 and indicate that learners most liked: 1. Interactive methods, 2. Hearing both Nurse and Doctor Perspectives, 3. Use of Cases, 4. Collaboration, 5. Relevant, Important and/or Practical Information , 6. Interdisciplinary/Interprofessional sessions and 7. Brief or Short sessions.
Conclusions: We implemented a Nurse-Doctor Co-Teaching series which received uniformly excellent overall ratings from nurse and resident learners. Learners particularly appreciated the interactive methods and the opportunity to hear both nurse and physician perspectives on common clinical situations. We found a significant improvement (p=0.01) in nurse comfort in communicating with a resident about an order following the co-teaching series, which may indicate better collaboration and communication among nurses and residents.