Background: Prior studies have found racial disparities in how patients are assessed for pain and prescribed opioids from emergency department and surgical settings. However, we do not know whether similar disparities exist among general medicine inpatients. We examined opioid prescriptions at discharge among adults admitted to the general medicine service at our medical center, with a focus on whether there were differences by race and ethnicity.
Methods: We identified all adults hospitalized on the general medicine service from 2012-2018 at a 600-bed urban academic teaching hospital. Using electronic health databases, we identified two cohorts of patients: first, patients who received opioids during their last 24 hours of hospitalization and second, all patients who were discharged with an opioid prescription, and collected data on their demographics, diagnoses codes, and medications. We excluded patients with diagnoses of cancer-related pain, sickle cell disease pain crises, patients discharged on hospice, or who were followed by palliative care. Patient self-reported race/ethnicity was categorized as White, Black, Hispanic (for patients who reported Hispanic ethnicity), Asian, or Other/Unknown. We used multivariable logistic regression to examine the likelihood of receiving an opioid prescription at discharge based on whether they had received opioids in the 24 hours prior to discharge. We then developed a second multivariable linear regression model, this time examining disparities in the total opioid days prescribed at discharge, calculated as the total morphine milligram equivalents (MME) prescribed divided by the MME administered during the last 24 hours of hospitalization. Models were adjusted for patient demographics (age, gender, limited English proficiency status), hospitalization factors (including length of stay, intensive care unit management, opioids received during the total stay and in the last 24 hours), and medical diagnoses (including adjusted Elixhauser comorbidity index and cancer).
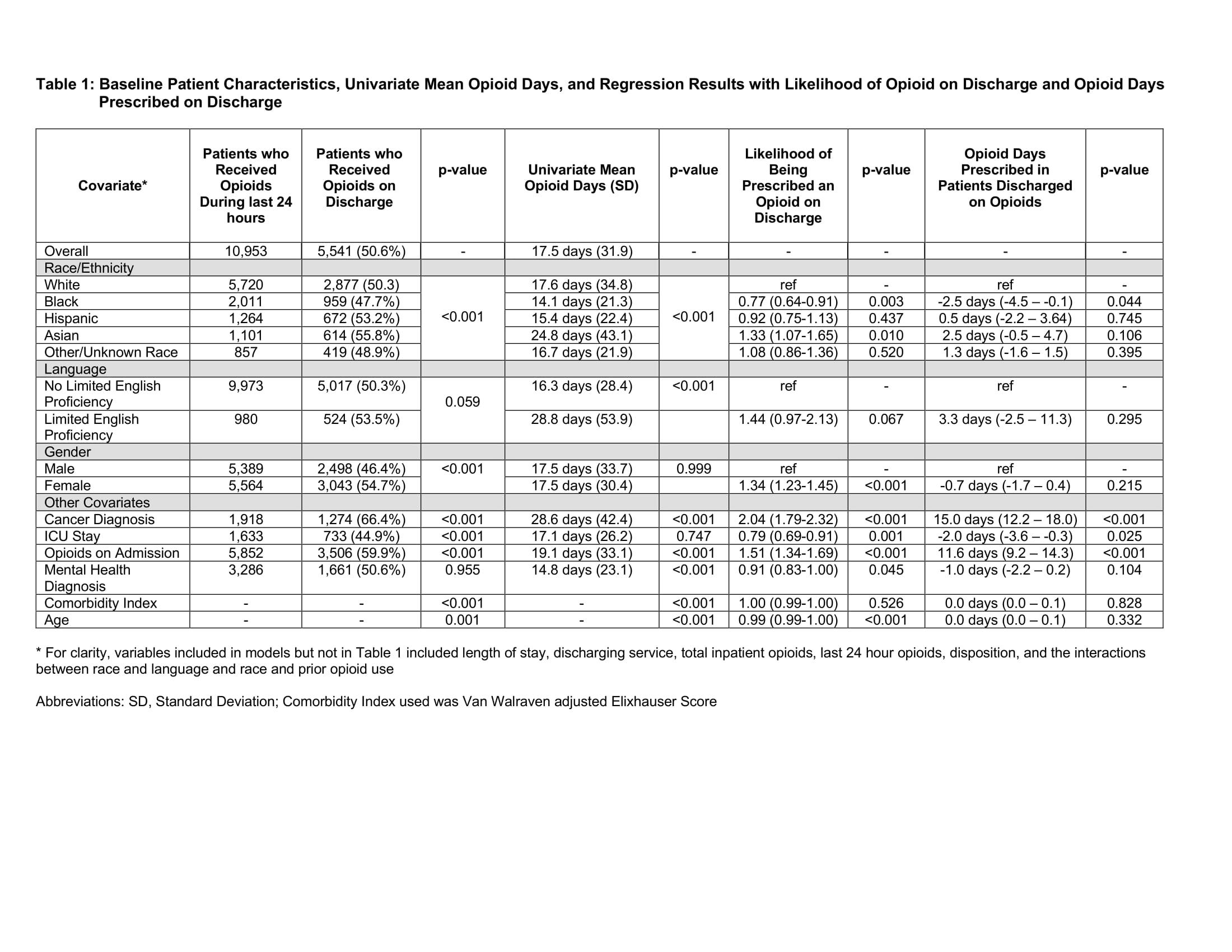
Results: We identified 10,953 patients who received opioids during the last 24 hours of hospitalization and 5,541 patients discharged on opioids. We found statistically significant differences by race/ethnicity in mean opioid days prescribed at discharge, in both univariate and multivariable analyses. In unadjusted univariate analysis, Black patients were prescribed fewer opioid days (14.1 days) compared to White patients (17.6 days). Adjusting for covariates, Black patients were less likely to receive opioids on discharge (OR 0.77, 95% CI 0.64 to 0.91) compared to White patients. Moreover, Black patients discharged on opioids received 2.5 fewer days of opioids (95% CI -4.5 to -0.1 days).
Conclusions: We found Black patients were less likely to be prescribed opioids on discharge. Black patients discharged on opioids received fewer days of opioids compared to other racial/ethnic groups.