Background: At the height of the spring 2020 COVID-19 pandemic in New York City, NYU Langone Hospital implemented visitor restrictions and NYU Grossman School of Medicine removed clerkship students from clinical rotations—both in an attempt to mitigate the spread of the virus. Frontline providers were busy delivering care to a surge of patients, leaving little time to administer daily updates to family members of hospitalized patients who were unable to visit their loved ones.
Purpose: The NYU Family Connect (NYUFC) program was created in an attempt to bridge this significant communication gap, delivering daily updates to family members of hospitalized COVID-19 patients and providing a mechanism for families to reach their family member’s care team. At the same time, the program allowed physicians, nurses, and other staff who were not treating COVID-19 patients (or who had reduced responsibilities) to contribute to the institution-wide response to the pandemic. It also empowered medical students to gain authentic training experiences while operating remotely.
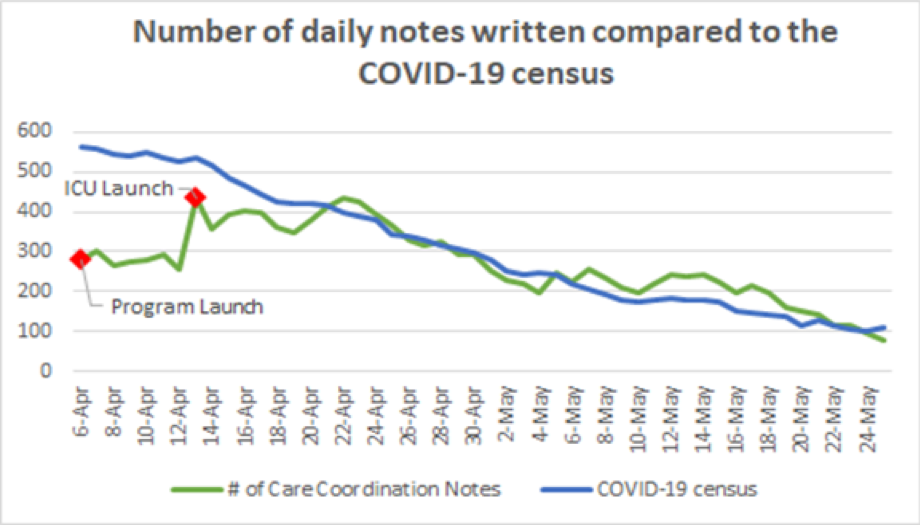
Description: NYUFC was a 3-part program operating from April 6th through June 25th, 2020 that impacted 1,800 families: (1) Proactive phone calls were made daily by medical student volunteers working remotely with mentoring attending physicians. Students and attendings were trained to obtain key information from patient charts, attend virtual rounds to ascertain the primary team’s daily plan for the patient, deliver pertinent clinical updates to patients’ family members via telephone calls, and document these telephone encounters in the electronic medical record. 115 medical students and 151 mentoring physicians participated in the program, following patients on both acute and intensive care units. Over the course of the COVID-19 surge at NYU Langone Health, 13,539 Care Coordination notes were documented in Epic and the program connected with the family member or health care proxy of every patient admitted between April 22nd and May 24th, 2020. (2) In-person continuity of the program was managed in the hospital by nurses who facilitated video visits between patients and families. They conducted over 1,000 video calls during this time. (3) A patient and family call center was created to triage all incoming calls to the hospital, managing over 16,000 calls. The 43 staff members who monitored the call center 24/7 answered non-clinical questions, documented and sent messages to care team members, and reduced the call volume going directly to the units.NYUFC participants and frontline providers were later surveyed, noting the utility and efficacy of the program. 88% of medical students who completed the survey felt that NYUFC was an important part of their medical education, citing their appreciation to remain involved in patient care during difficult times, to learn from physician mentors spanning many specialties, and to gain experience communicating with clinical teams, patients, and patients’ loved ones. Overall, frontline providers also found the program to be valuable, with 88% indicating that NYUFC provided a critical resource to families and 78% agreeing that the Care Coordination notes were important for patient care.
Conclusions: NYUFC served a vital role during unprecedented times, facilitating relief for frontline providers and empowering medical students to participate in novel patient care. Most importantly, it ensured daily, compassionate updates to families whose loved ones were hospitalized with COVID-19.