Background: The obesity paradox describes a counterintuitive observation of improved outcomes in patients with obesity. Analysis of the association among overweight/obesity and leading causes of inpatient mortality in a systemic manner has not been conducted.
Methods: We used STATA (StataCorp, College Station, Texas) to analyze the 2016 National Inpatient Sample (NIS). We recognized patients with underweight, overweight, obesity class I, obesity class II, and obesity class III, using BMI-related International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes. We identified ten leading inpatient-death-associated principle diagnoses using ICD-10-CM codes. We used multivariable logistic regression to calculate the odds ratio adjusting the following confounding factors: age, gender, race, smoking, comorbidities (Charlson comorbidity index), income (median household income for patient’s ZIP Code), income, hospital location (urban or rural), region, teaching status, and bed size. We used a p-value less than 0.05 as the threshold of statistical significance.
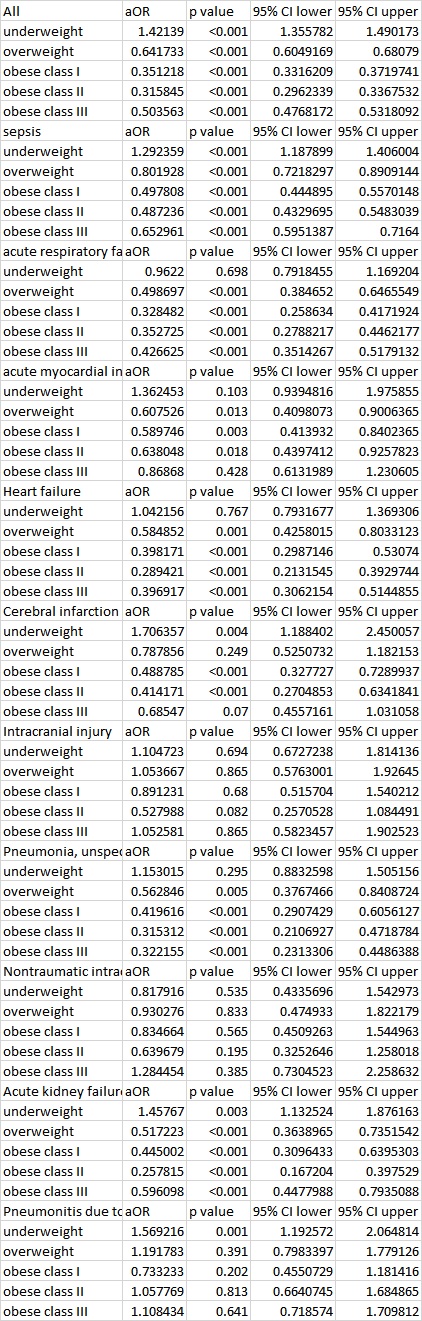
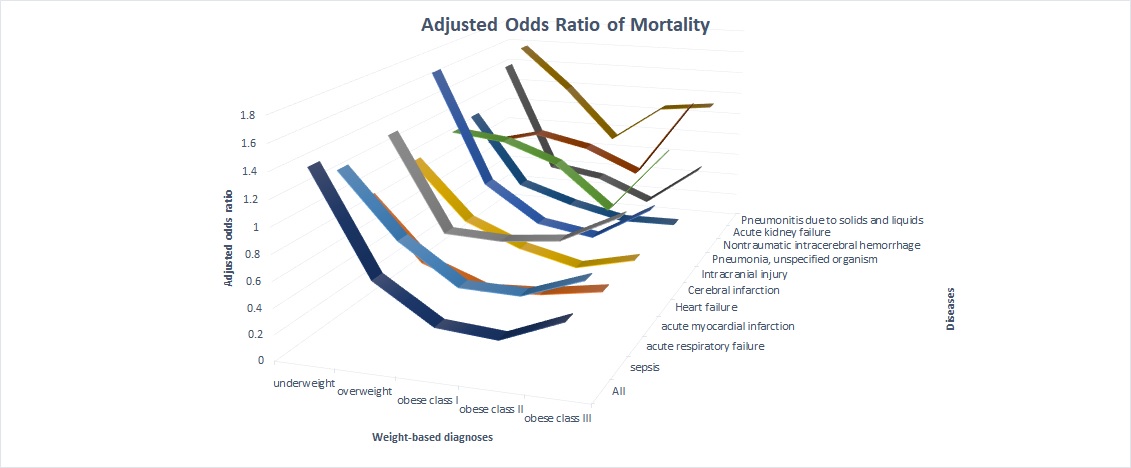
Results: National Inpatient Sample (NIS) contains an estimate of 35,675,421 inpatient admissions in the United States (U.S.) in the year of 2016, among which 5,162,782 admissions had body mass index (BMI) charted as secondary diagnoses. Overall, underweight was associated with higher odds of mortality [adjusted odds ratio (aOR): 1.42; p <0.001], and overweight, obesity class I, class II, and class III were associated with lower odds of mortality (aOR: 0.64, 0.35, 0.32, and 0.50, respectively; all p<0.001). We identified ten leading inpatient-death-associated principle diagnoses: sepsis (estimated number of admissions: 1,819,014), respiratory failure (469,455), acute myocardial infarction (647,374), heart failure (809,374), cerebral infarction (509,215), intracranial injury (210,225), pneumonia (625,564), nontraumatic intracerebral hemorrhage (70,750), acute kidney failure (529,870), and aspiration pneumonitis (153,690). Among these diagnoses, an obesity paradox with statistical significance existed in sepsis, acute respiratory failure, acute myocardial infarction, heart failure, cerebral infarction, pneumonia, and acute kidney failure. Admissions with principal diagnoses of intracranial injury, nontraumatic intracranial bleeding, and aspiration pneumonitis did not demonstrate an obesity paradox.
Conclusions: Obesity paradoxes were observed in seven out of ten leading inpatient-death-associated principal diagnoses. The reason why the obesity paradox existed or did not exist in certain diseases is not clear. Out of the three diagnoses unrelated to obesity paradoxes, two were mechanical injuries, suggesting that the underlying mechanism of obesity paradox is likely internal.