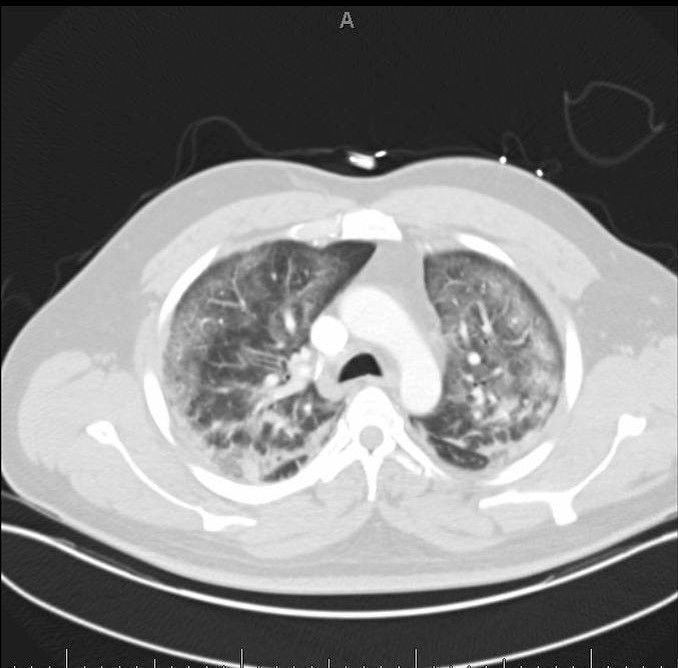
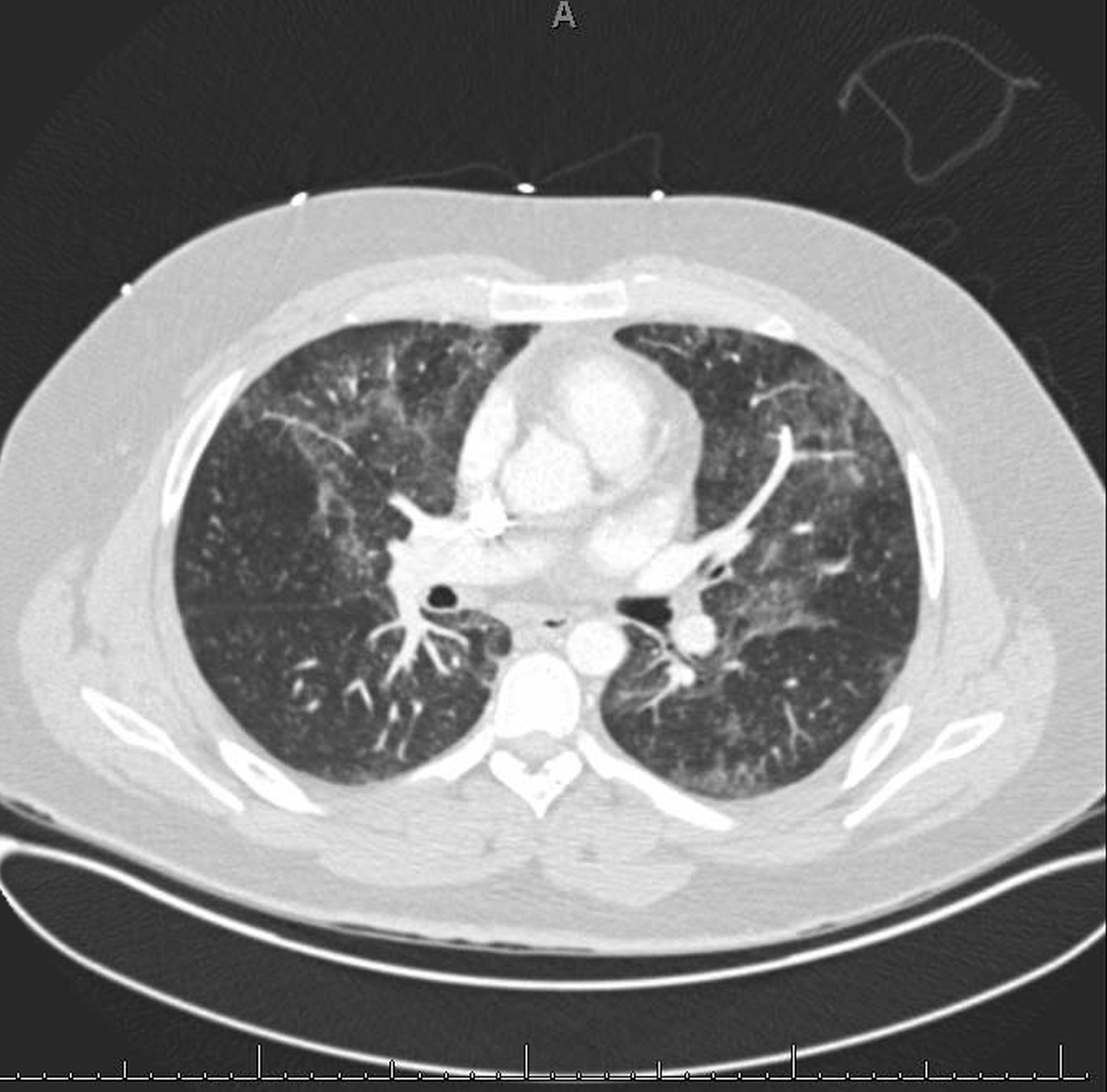
Case Presentation: Case I:A 45-year-old male with a past medical history of vaping marijuana and nicotine presented with a four-day history of progressive dyspnea associated with cough, fevers, fatigue, weight loss, and diarrhea. He was found to be hypoxic to 72% oxygen saturation with a new 15-liter (L) oxygen requirement and febrile to 38.5 Celsius. Radiology demonstrating bilateral symmetric lung opacities, bronchiectasis, and mediastinal lymphadenopathy with posterior consolidation. He was intubated, started on vasopressors, and transferred to the intensive care unit (ICU) eventually required tracheostomy placement due to prolonged intubation. After 3 weeks in the hospital, he was discharged home without supplemental oxygen. Case II:A 23-year old male with a history of schizophrenia presented with a 1-week history of nausea, vomiting, diarrhea, diffuse abdominal pain, weight loss along with a 3-day history of fever, chills, productive cough, dyspnea, and orthopnea with history of 3 months of vaping nicotine with no recreational drug use. On admission, he was febrile to 38.3 and was found to be hypoxic requiring 15L 02 on non-rebreather. ABG showed severe hypoxemia with PO2 of 43 on 15 liters non-rebreather. Chest CT showed multifocal regions of centrilobular ground-glass and reticular opacities involving all 5 lobes with scattered bronchial wall thickening. He was transferred to the ICU requiring BIPAP. He improved with conservative management and was discharged home on oxygen with follow up by pulmonary. In both of the above cases extensive infectious workup including blood cultures, sputum cultures, urine streptococcus, parasite stool/ova, respiratory panel, vasculitis panel, 1,3 beta D glucan, TB, CMV, HSV and HIV screen was all negative. TTE was performed to rule out cardiac etiology and was normal. In both of the above cases, the patients were treated with empirical IV antibiotics for CAP and 5 days course of IV steroids.
Discussion: As of October 29, 2019, 1,888 cases of e-cigarette associated lung injury cases have been reported to the CDC with 36 reported deaths. Approximately 80% of described cases are associated with the use of both nicotine and tetrahydrocannabinol products. Electronic cigarettes (e-cigarettes) have become a popular alternative to conventional cigarettes. Though considered safer than cigarettes, the acute and long-term effects of vaping are not well understood. Little is known as to how e-cigarettes cause lung injury, however depending on the type of chemical agent and the amount of material inhaled, patients may experience symptoms ranging from nausea, vomiting, abdominal pain, diarrhea, fever, chills, and weight loss to respiratory tract discomfort to acute airway injury with pneumonitis and damage to the parenchyma, alveolar edema, respiratory failure, and death. The CDC has recently named this combination of symptoms EVALI. A common pathophysiological pathway includes alveolar inflammation with associated airway edema and epithelial sloughing. EVALI demonstrates different pneumonitis patterns. Recent reports suggest vitamin E acetate association with EVALI.
Conclusions: These cases illustrate that e-cigarettes are associated with significant morbidity. EVALI an epidemic that requires special attention from physicians, as well as increased public awareness of the harmful effects associated with e-cigarettes. Finally, it is important that physicians educate their patients that vaping is not a harmless alternative to smoking tobacco.