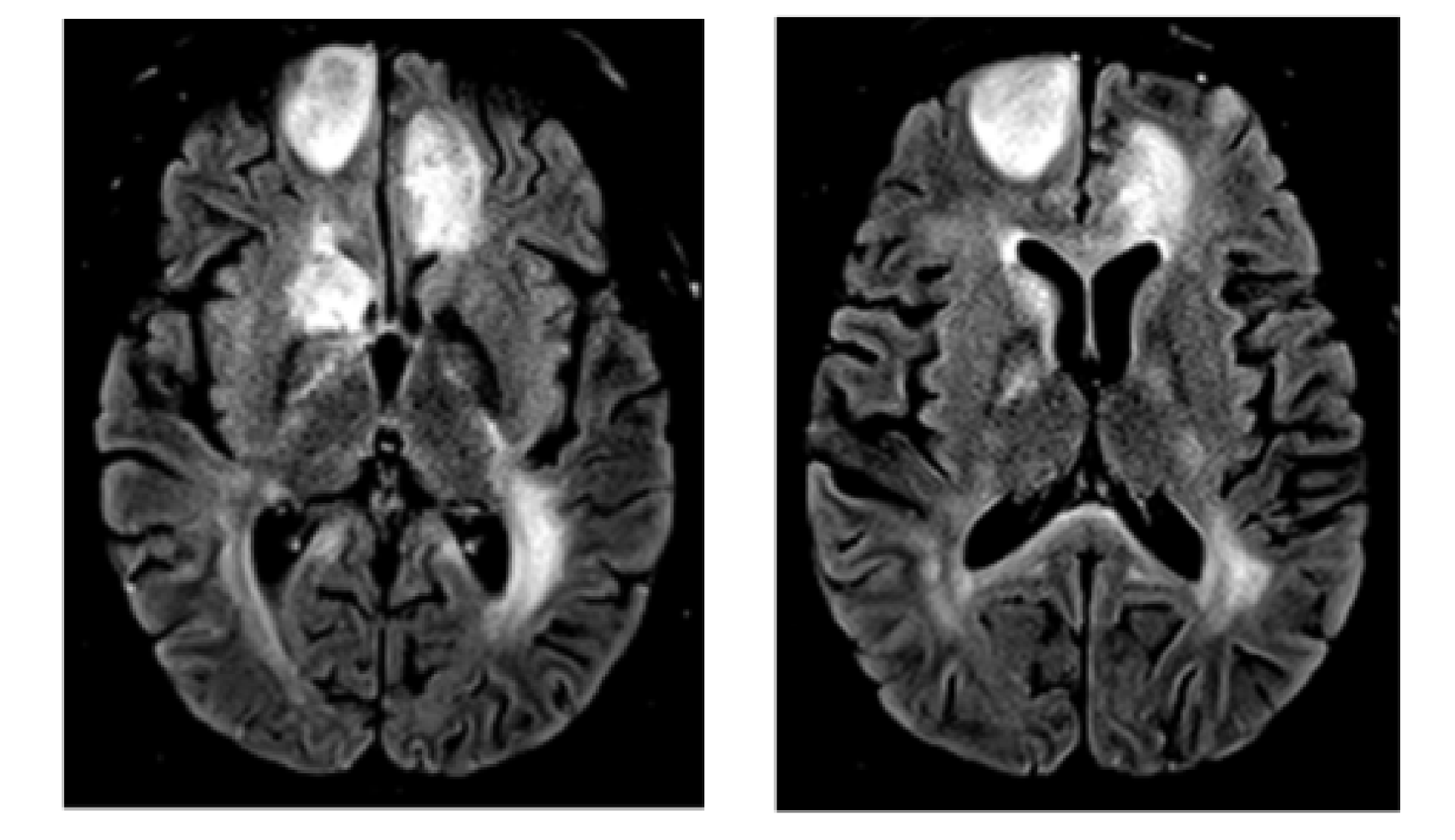
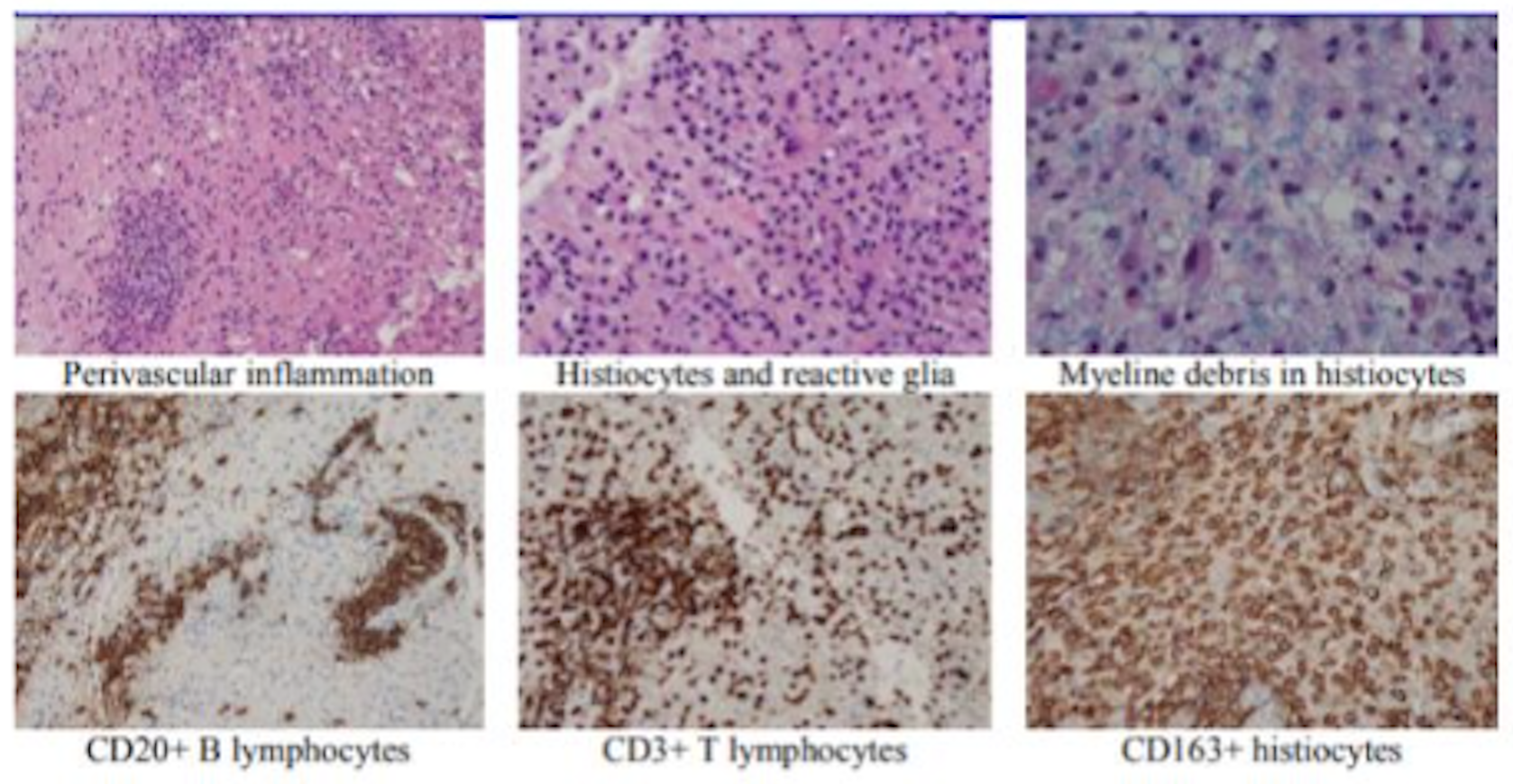
Case Presentation: A 41-year-old female with Acquired Immunodeficiency Syndrome (AIDS) presented with a complex clinical picture involving seizures, falls, and fever. Limited historical information hindered a comprehensive understanding of the patient’s medical background. Upon examination, the patient exhibited signs of cachexia, lethargy, and distinctive skin lesions. Laboratory results revealed anemia, leukocytosis, and a significantly low CD4 count. Dark, pigmented lesions were observed on the lower extremities, face, and upper chest.Magnetic resonance imaging (MRI) of the brain, disclosed heterogeneously enhancing mass-like lesions in the bilateral frontal lobes and right basal ganglia (Figure 1). Laboratory analysis of cerebrospinal fluid identified cytomegalovirus (CMV) positivity. Empirical treatment ensued, involving broad-spectrum antibiotics, anti-CMV medications, and prophylactic agents due to the patient’s compromised immune status. Early management involved a broad-spectrum approach, with antibiotics and anti-CMV medications initiated based on initial findings. Prophylactic agents were administered to address potential opportunistic infections.Given the complexity of the presentation, a stereotactic brain biopsy was performed by neurosurgery. The biopsy excluded primary CNS lymphoma but uncovered features consistent with Epstein-Barr virus (EBV)-associated B-cell Lymphoproliferative Disorder (figure2). The final diagnosis centered on known association of EBV-associated B-cell Lymphoproliferative Disorder in AIDS with distinctive morphology. As the diagnostic picture clarified, treatment was refined to align with the specific diagnosis. The patient’s condition improved, leading to successful extubation and discharge with a tailored ART regimen.
Discussion: Our case highlights that CMV in Cerebrospinal fluid testing is not definitive in patients with AIDS. The distinctive features of CMV periventricular lesions were not seen and with heterogeneously enhancing mass like lesions prompted further workup getting brain biopsy. EBV, a gamma Herpesvirus, poses a heightened risk for lymphomagenesis in HIV patients, contributing significantly to mortality in untreated cases. Known for associations with Burkitt’s lymphoma, classic Hodgkin’s lymphoma, and immunocompromised lymphomas, EBV’s impact involves B-cell immortalization, MYC protein dysregulation, and cytokine-induced B-cell proliferation. Notably, HIV-associated diffuse large B-cell lymphoma frequently involves the brain, emphasizing the importance of vigilance for neurological symptoms in AIDS patients. Concurrently, our case highlights the presence of CMV in AIDS patients, emphasizing the need for timely recognition and treatment, particularly at lower CMV viremia thresholds for expedited clearance. Understanding these viral interactions is paramount for effective management, timely interventions, and improved outcomes in the complex landscape of HIV/AIDS-related lymphoproliferative disorders.
Conclusions: This case illuminates the critical role of EBV in lymphoproliferative disorders within AIDS. Typical morphologic features and atypical presentation for CMV lead to further work up. The collaboration of neurological imaging, CSF analysis, and a stereotactic brain biopsy proved instrumental in uncovering the underlying EBV-associated B-cell Lymphoproliferative Disorder.