Background: Improving hospital throughput and capacity is a challenge that many health systems face. Specifically, emergency room overcrowding leads to delayed access to treatment and increased mortality, thereby negatively impacting patient safety (Franklin, et al., 2023). Health systems strive to employ multiple strategies to tackle the issues around patient flow. One such strategy includes the development of a clinical command center whose principal function is to oversee and facilitate patient flow from within and into the health system. The role and impact of the hospitalist within the clinical command center is yet to be evaluated.
Purpose: We describe the purpose and role of a central hospitalist (CH) within the clinical command center at an urban academic health system.
Description: The CH responsibilities include collaborating with the clinical command center and local team to determine appropriateness of internal and external patient transfers across the system, referring patients for admission into Hospital at Home program, and reviewing and implementing sepsis alerts within the health system. We reviewed data extracted from our electronic medical record and then reported in an analytics platform to evaluate the impact of the central hospitalist on system-wide hospital throughput.
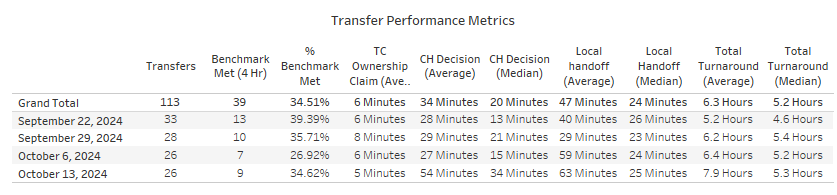
Conclusions: Over 5000 cases have been reviewed by the central hospitalist and transferred within or into the health system since 2022. Level-loading cases, which account for the majority of the transfers, are patients who were transferred out of one of our over-crowded emergency rooms directly to an inpatient bed at one of our other hospitals within the system. Our data shows that post implementation of the central hospitalist program, level-load transfers have resulted in a reduction in ED boarding time (-15.76hours), average length of stay (-1.8 days), and excess days (-2041 days) leading to an increase in additional bed capacity for admissions (+256 admissions). Currently average CH decision time, which is defined as time from initial contact by clinical command center to disposition decision, is 34 minutes (average) and 20 minutes (median) which is near goal of < 30 minutes over a 1 month period and has significantly improved from pre-implementation decision time of over 100 minutes.The impact of the central hospitalist role within the clinical command center shows clear value with improved patient flow and throughput within the system. We suggest that the hospitalist plays a vital role within the clinical command center, acting as a safety net to ensure appropriateness of transfers and providing clinical oversight throughout the health system.