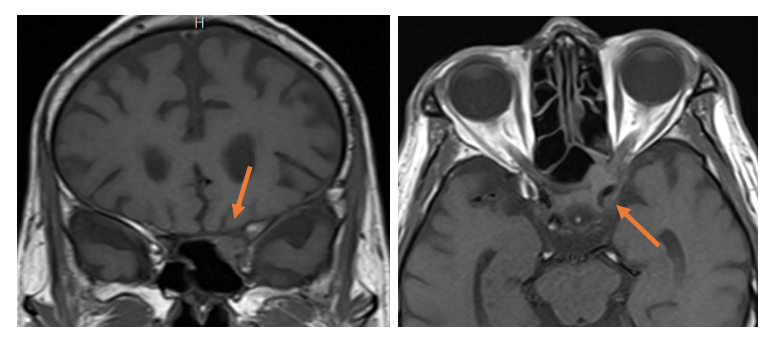
Case Presentation: An 80- year old immunocompetent Vietnamese man with hypertension, atrial fibrillation, and prostate cancer in remission was admitted for progressive vision loss and headaches. 6 weeks before presentation he began to have persistent, disabling left fronto-temporal headaches. 2 weeks prior he developed sudden left sided vision loss. Outpatient left temporal artery biopsy was negative for arteritis. One week prior he had worsening left and new onset right vision loss. He had 5 lb weight loss but no fevers, jaw claudication, eye pain or redness, focal weakness, or joint pains. On admission he had normal ocular movements, right visual acuity of 20/60, left no light perception, and no optic nerve edema or retinal pathology. Left sided scalp tenderness was noted. CBC, CMP, ESR, CRP, lumbar puncture, serum aspergillus galactomannan, serum/CSF NMO, RPR, HIV, ANCA, and ANA were all normal. MRI brain and orbits showed a T2 hyperintense signal of left intraorbital optic nerve without associated enhancement.High dose steroids for giant cell arteritis or other posterior optic neuropathy were started. Patient noted partial improvement in headache and right eye vision. He underwent temporal artery biopsy on contralateral right side which was negative for arteritis.We had neuro-ophthalmology review radiology on fourth hospital day. They noted previously overlooked T1/T2 hypointense foci in left anterior cavernous sinus/orbital apex (Image 1). CT of sinuses showed extension into the sella, left optic canal, and sphenoid osseous erosion. Pathology from trans-nasal biopsy showed tissue invasive fungal process with necrosis and abscess. Cultures grew both Aspergillus fumigatus and drug resistant Staphylococcus epidermidis.We diagnosed localized invasive sino-orbital aspergillosis complicated by secondary bacterial infection. He received six weeks of IV Vancomycin and planned twelve-month course of oral voriconazole. At two-month follow-up patient had resolution of headaches, improvement in right sided vision, but continued blindness in his left eye.
Discussion: Aspergillus normally colonizes the aero-digestive tract and pathogenicity in immunocompetent patients is rare. Orbital involvement occurs by contiguous spread from the paranasal sinuses (Adulkar 2019). We had initial suspicion for giant cell arteritis given the temporal headache and vision loss in an 80-year-old man. We suffered from availability bias. The normal temporal artery biopsy and negative inflammatory markers were discrepant features. Common signs and symptoms of orbital aspergillosis are proptosis, pain located on one side of the head or retrobulbar area, disorders of eye movements, and decreased vision. Misdiagnosis of optic neuritis, temporal arteritis, malignant tumor, idiopathic orbital inflammation, and Tolosa-Hunt syndrome frequently occurs (Kawakami 2017). Corticosteroids can potentially lead to initial improvement, but their use increases risk of complications (Ali 2013).
Conclusions: Sino-invasive orbital aspergillosis is potentially life-threatening. It can occur in immunocompetent individuals. Sutton’s law is a heuristic named after Willie Sutton who, when asked why he robbed banks, replied “Because that’s where the money is!” Our case demonstrates the opposite; “Sutton’s slip,” which occurs when possibilities other than obvious are prematurely closed. When an ocular condition has atypical features be prepared to cast a broad net because timely diagnosis can be vision saving.