Background: In 2019, the US Food & Drug Administration issued a warning regarding safety of gabapentin use in patients with respiratory conditions, including chronic obstructive pulmonary disease (COPD). Gabapentin is widely prescribed, often for off-label indications, however limited data exist regarding safety and outcomes among patients with COPD.
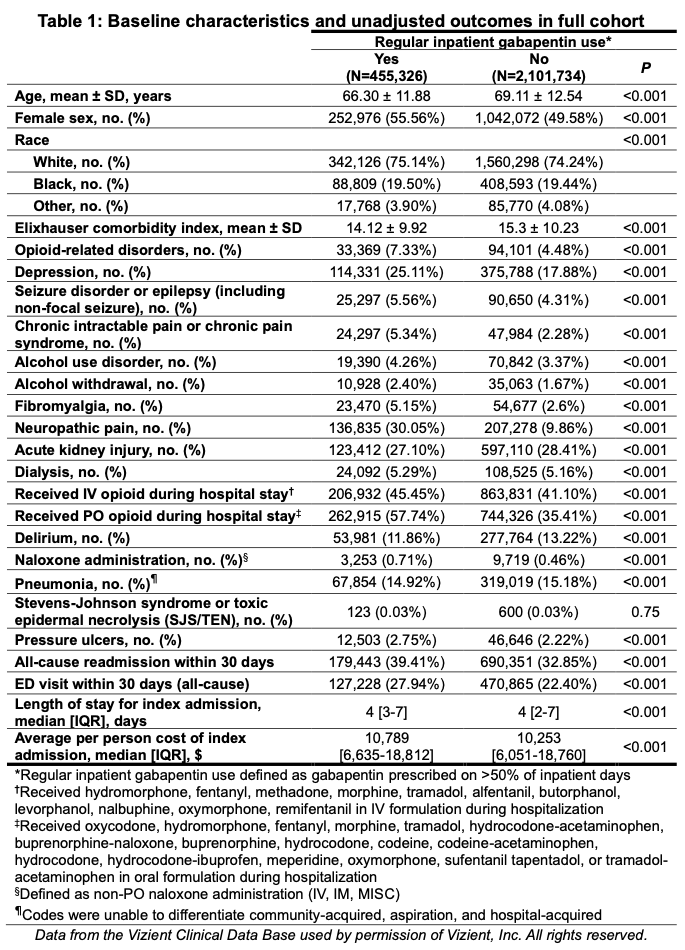
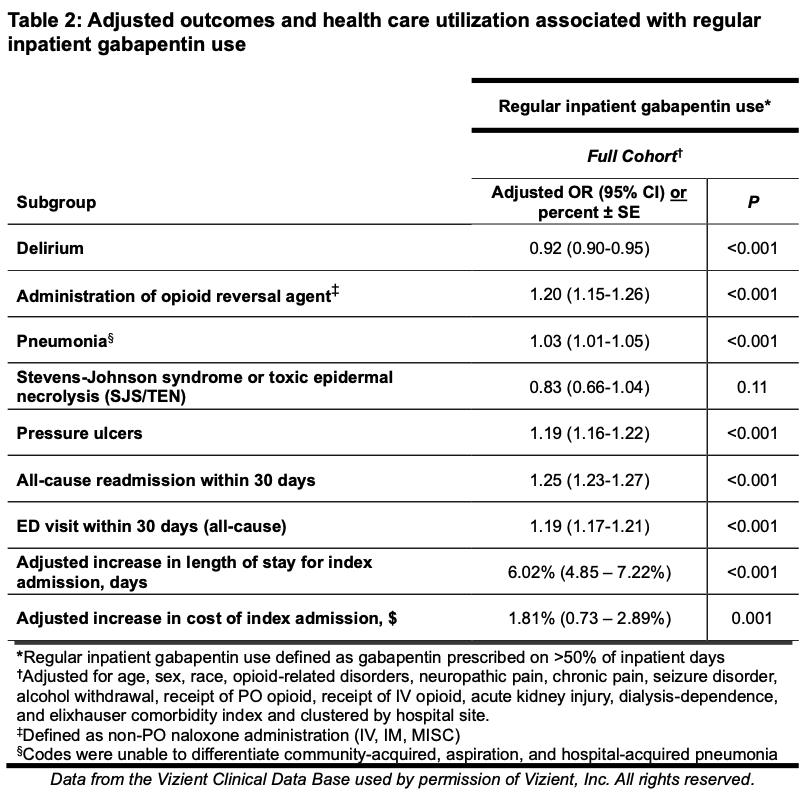
Methods: We analyzed data from 29 US hospitals that submit administrative billing data to the Vizient Clinical Database. Billing data were used to characterize patient demographics and ICD-10 codes J41.XX through J44.XX were used to define our COPD patient cohort. Inpatient gabapentin exposure was defined as having pharmacy charges for gabapentin documented on >50% of a patient’s hospital days. Additional baseline comorbidities and outcomes of interest (such as pneumonia and delirium) were determined by ICD-10 codes. We used chi-squared tests, t-tests, and Wilcoxon ranksum tests to compare characteristics among patients with and without regular inpatient gabapentin use during an index hospitalization. Primary analyses were conducted using multivariable logistic regression and multivariable linear regression of log-transformed length-of-stay and cost data.
Results: A total of 2,557,060 inpatients (mean age 68.61 ± 12.47, 50.65% female) with COPD were included. Of 523,880 COPD patients who received any inpatient gabapentin, 455,326 received gabapentin on >50% of hospital days (86.91% of gabapentin recipients; 17.81% of full cohort). Delirium (11.86% vs. 13.22%, p< 0.001) and pneumonia (14.92% vs. 15.18%, p< 0.001) were less common among patients with regular inpatient gabapentin use, while naloxone administration (0.71% vs. 0.46%, p< 0.001), subsequent 30-day ED visits (27.94% vs. 22.40%, p< 0.001), and 30-day all-cause readmissions (39.41% vs. 32.85%, p< 0.001) were more common among patients with regular inpatient gabapentin use. After multivariable logistic regression adjusting for comorbid conditions and common indications for gabapentin (e.g. neuropathic pain), regular gabapentin use was associated with lower odds of delirium (aOR 0.92, 95% CI 0.90-0.95) but higher odds of pneumonia (aOR 1.03, 95% CI 1.01-1.05), opioid reversal agent administration (aOR 1.20, 95% CI 1.15-1.26), 30-day ED visits (aOR 1.19, 95% CI 1.17-1.21), and 30-day readmissions (aOR 1.25, 95% CI 1.23-1.27). In the full cohort, the median length of stay was 4 days (IQR 2 - 7) and median cost of admission was $10,355 (IQR 6,155 – 18,770) per patient. Regular inpatient gabapentin use was associated with a 6.02% (95% CI 4.85-7.22%) increase in adjusted length of stay and 1.81% (95% CI 0.73-2.89%) increase in adjusted cost of index admission.
Conclusions: In this large cohort of hospitalized adults with COPD, most patients who received inpatient gabapentin received it on more than half of hospital days, and regular inpatient use of gabapentin appeared to be associated with higher inpatient resource use and worse post-acute outcomes. Though use of gabapentin in the hospital is often driven by longer-term care patterns, our data suggest that exposure to gabapentin in patients hospitalized with COPD may have meaningful implications for patients and health systems.