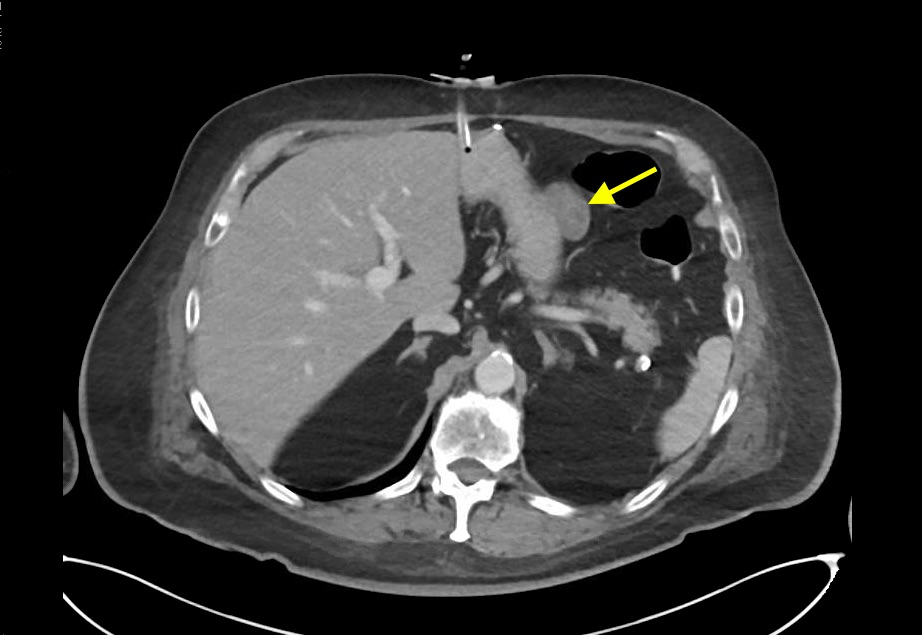
Case Presentation: An 84-year-old Caucasian male with a history of hyperlipidemia presented to his primary care provider with a 6-week history of an erythematous rash with associated proximal limb weakness but without complaint of breathing or swallowing difficulties. Statin-induced rash with myopathy were suspected so his statin was stopped, and he was referred for skin biopsy. It revealed histology consistent with dermatomyositis (DM) and he was started on a Prednisone taper. Upon its completion, the rash had improved, but his proximal limb weakness had not and he began to complain of difficulty swallowing. He was sent to the ED for further evaluation. The rash was in a shawl-like distribution. Periorbital edema, cutaneous ulceration, Gottron’s papules, and periungual erythema were also present. Proximal muscle weakness of the upper and lower extremities was symmetric and graded 2/5. CK was 1869U/L (normal rage 39-308U/L) and ESR 22 mm/h (normal range 3-10mm/h). ANA titer was elevated at 1:1280 but dsDNA was negative and complement levels were normal. Myositis antibody screen was negative for anti-Jo-1, mitochondrial Ab, and smooth muscle Ab. CT imaging identified a cystic mass along the outer aspect of the greater curvature of the stomach, which biopsy confirmed to be a spindle cell type gastrointestinal stromal tumor (GIST) immunoreactive for CD115 and negative for desmin and S100. PET scan did not identify metastatic disease. Systemic treatment with pulse dose steroids failed to improve his symptoms and CK trend, which prompted initiation of IVIG. He responded to this and Methotrexate was initiated as maintenance therapy. Oncology recommended neoadjuvant Imatinib to treat the localized GIST tumor. The patient developed septic shock due to aspiration pneumonia on day 29 of admission and required pressor support and intubation. Immunosuppressive therapy was halted, but the patient was unable to be weaned off of the ventilator. After 2 weeks in the ICU, the patient’s family elected to pursue comfort care and the patient died on hospital day 47.
Discussion: The most updated diagnostic criteria for the idiopathic inflammatory myopathies (IIMs) would have diagnosed our patient with dermatomyositis (DM) sooner and without the need for pathology. Additionally, earlier appreciation of the patient’s cutaneous ulceration as a poor prognostic indicator may also have led to more aggressive interventions sooner. Our patient failed to respond to IV steroids and while he ultimately did respond to IVIG, time was lost and his dysphagia worsened, which served to increase his aspiration risk. While DM caused by a GIST is rare, its prognosis is excellent, if localized. Had our patient not aspirated and developed septic shock, he stood a good chance at recovery given the absence of metastatic disease.
Conclusions: Additional research into the risk stratification of patients with DM may allow for earlier and more effective treatment. Emerging evidence suggests that DM with cutaneous ulceration is associated with a more severe disease course and a poor response to immunosuppressive therapies and may require high-dose steroids, IVIG, and other disease-modifying antirheumatic drugs. Dermatomyositis has a strong association with malignancy, and the importance of screening for it early cannot be overstated. When malignancy is found, the prognosis is generally poor, but localized, low grade GIST carries an excellent prognosis and is treated with tyrosine kinase inhibitors such as imatinib. Response rates can exceed 90%.