Case Presentation: A 66-year old woman was receiving I.V. iron at an infusion center when she developed dyspnea, weakness, nausea, and fever. In the ED, she was hypotensive to 77/56 mmHg (baseline 110s systolic), heart rate 126 bpm, respirations 19/min. Her husband reported she’d been scratched by her cat one day prior. Medical history was notable for congestive heart failure, COPD, atrial fibrillation, pulmonary hypertension, and hemorrhagic hereditary telangiectasia (Oslo Weber Rendu syndrome).
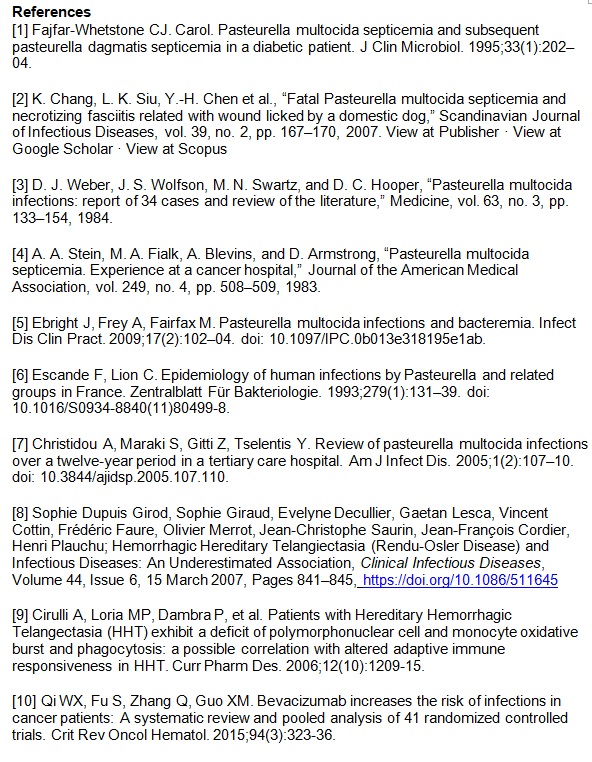
On physical examination, she had a 4 cm laceration and 1 cm puncture wound on the right inner shin and 4 cm laceration on the right outer tibia area (Fig 1). Patient was jaundiced per her baseline.
ECG showed atrial flutter and later atrial fibrillation with RVR. Blood tests showed WBC of 29.9 K/ul with ANC 27.2 K/ul, hemoglobin 10.8 g/dL, creatinine 2.1 mg/dL (baseline 1.2), and elevated bilirubin 8 mg/dL (baseline 4-7, fluctuating) with direct bilirubin 4.50 mg/dL. Chest X-ray was only significant for cardiomegaly.
In the ICU she was started on I.V. vancomycin and piperacillin-tazobactam. She was started on norepinephrine to maintain blood pressure. For chronic GI bleed secondary to HHT, her home dose of octreotide was continued. Atrial fibrillation with RVR was controlled with amiodarone.
Two of 4 blood cultures grew gram negative bacilli later speciated as Pasteurella multocida susceptible to ceftriaxone. The patient was weaned off norepinephrine with normalization of all vital signs throughout the 5-day hospital course. She was discharged in good condition with continuation of I.V. ceftriaxone for 2 more weeks.
Discussion: Pasteurella multocida is a gram negative coccobacillus with a high carriage rate amongst pets (1-2). It commonly causes cellulitis via direct inoculation by animal scratch. In immunocompromised, elderly, or pediatric patients it can cause respiratory disease, meningitis, sepsis, and bacteremia, with high fatality rates (3-7). More severe presentations are seen in patients with COPD, cirrhosis, or on dialysis. Patients with HHT have an increased burden of infectious disease (8-9). Our patient was on bevacizumab (Avastin); one meta-analysis (10) associated bevacizumab with a higher rate of febrile neutropenia in cancer patients, although subgroup analyses did not stratify patients who were only receiving bevacizumab alone.
Conclusions: This case demonstrates that HHT and bevacizumab use can be additional risk factors for developing Pasteurella bacteremia. From an inpatient perspective, such patients should be treated empirically for gram negative bacteremia even if initial presentation is cellulitis from an animal scratch without signs of systemic inflammatory response (SIRS) (References: Table 1).
.jpg)