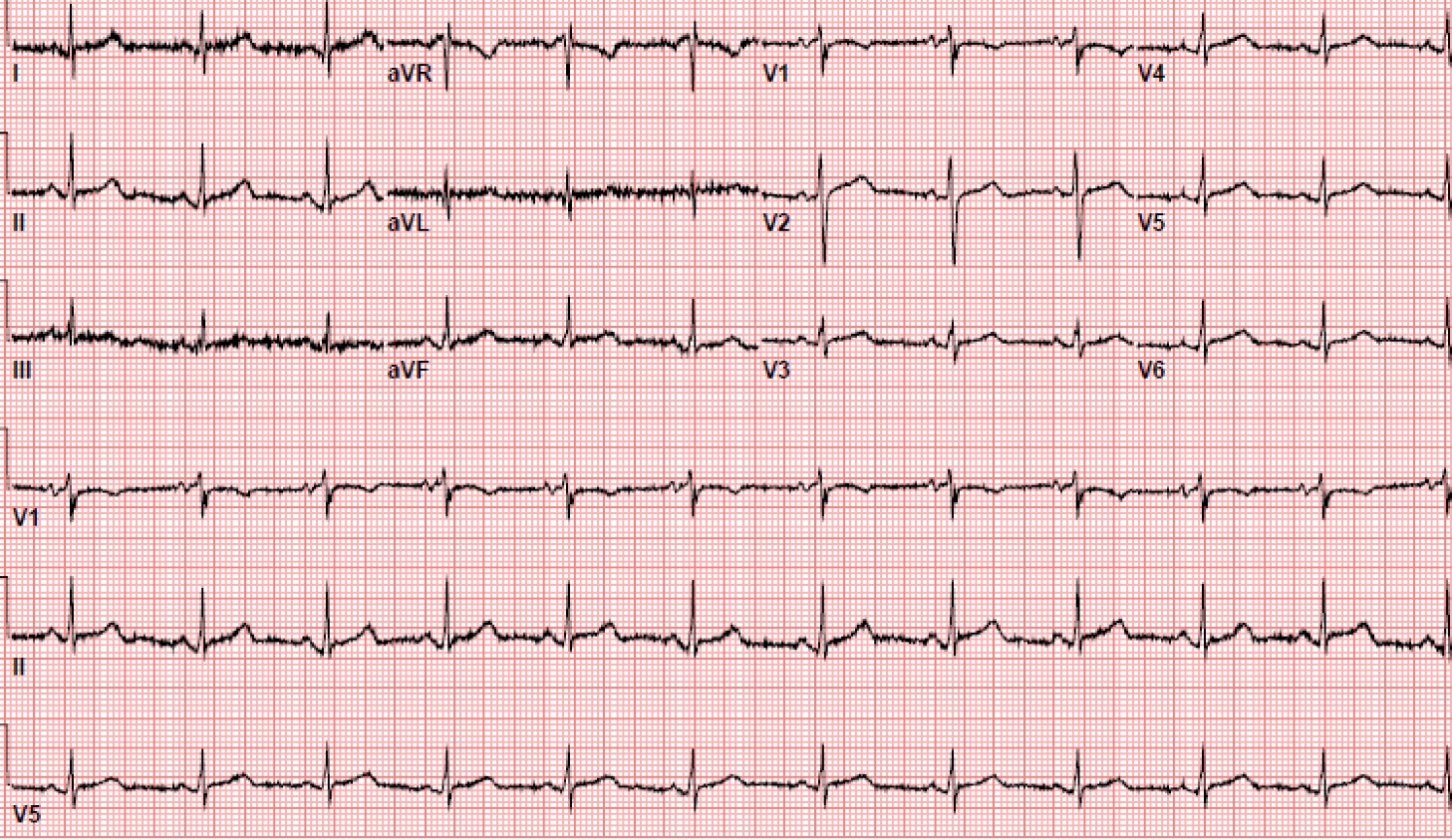
Case Presentation: A 70 year-old female with hypertension and diabetes presented to the hospital with a one-day history of non-positional, left-sided chest pain associated with shortness of breath and subjective fevers. Physical exam and vitals were unremarkable. Work up included three negative troponins, EKG in normal sinus rhythm (Figure 1), and D-Dimer of 1100 ng/mL. CTA chest revealed a right subsegmental middle lobe filling defect consistent with pulmonary embolism for which patient was initiated on anticoagulation with resolution of chest pain.
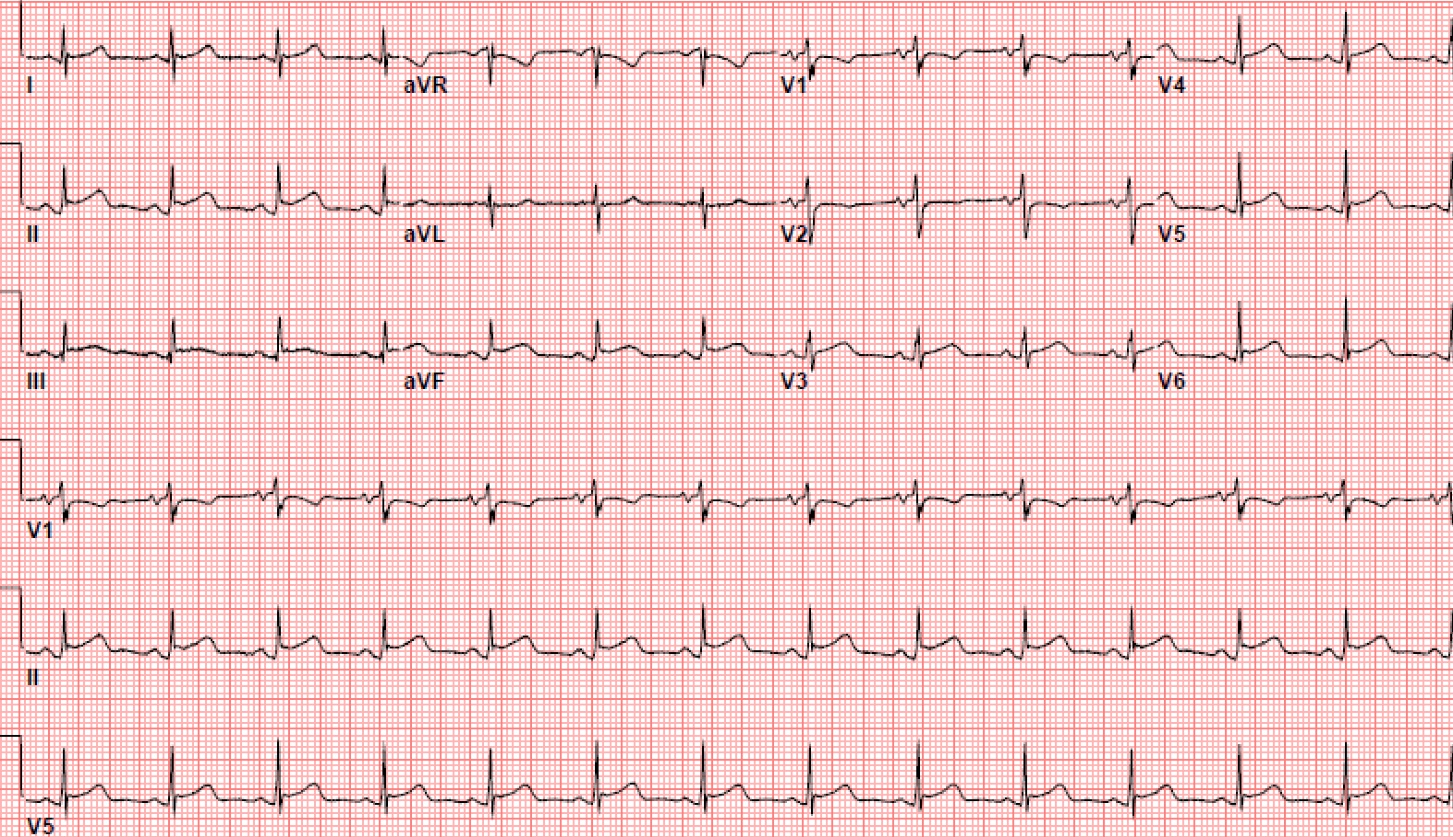
Approximately 24 hours after initial presentation the patient reported a new chest pain described as sharp, pleuritic, worse with lying flat and improved with sitting forward. Vitals revealed fever to 100.5 F. Repeat EKG demonstrated diffuse ST elevations (Figure 2). Labs showed a negative troponin and ESR and CRP at 63 mm/hr and >190 mg/L, respectively. Echo showed a trace pericardial effusion, normal ejection fraction, and no evidence of right heart strain. The patient was diagnosed with acute pericarditis and initiated on colchicine and NSAIDs with resolution of symptoms.
Common causes for pericarditis including viral URI, TB, connective tissue disorders, and malignancy were ruled out with a negative review of symptoms, subsequent laboratory analysis and additional history from the patient’s primary care provider. Given the unlikeliness of other etiologies, her acute pericarditis was felt to be secondary to her pulmonary embolism.
Discussion: Between 80-90% of pericarditis cases are idiopathic or presumed to be of viral etiology. Given the relatively benign course of the majority of causes of pericarditis a definitive work up is often not performed. However, this case highlights an additional “can’t miss” cause of pericarditis – pulmonary embolism. Although rare, post-pulmonary embolism pericarditis is a well-documented phenomenon associated with elevated ESR, CRP, and low-grade fevers as in this patient’s presentation. Proposed mechanisms include increased friction of an enlarged pulmonary artery and right ventricle against the pericardium and an immunologic response, similar to Dressler syndrome.
Conclusions: Despite being a known cause of pericarditis, pulmonary embolism is frequently overlooked or completely excluded from clinicians’ differentials. Although the exact cause of pericarditis is often unknown, in patients with idiopathic pericarditis with no infectious signs, pulmonary embolism should always be considered based on history and physical exam findings to avoid missing a “can’t miss” diagnosis.