Background: The hospital setting can be stressful for both patients and providers. The lingering effects of the COVID-19 pandemic such as staffing shortages, hospital overcrowding, and provider burnout have only exacerbated this problem. In 2023, we undertook a study aimed at improving the wellness of both patients and providers. Data gathered from this study will help us develop innovative, patient-centered, and holistic approaches to care that focus on the emotional, social, relational, and spiritual needs of patients. Recently, the Veterans Health Administration has implemented such a “Whole Health” program nationally, which includes activities such as mindfulness, massage therapy, yoga, and tai chi.
Methods: To better understand patient views and experiences, we conducted patient journeys at two Midwestern hospitals. These journeys, adapted from an engineering concept called Customer Journeys, included observing patients throughout their hospitalization and conducting follow-up interviews after discharge. During observations, study staff were positioned outside of patient rooms and monitored activity throughout the day. Information related to how patients spent their time was captured via notetaking (including time stamps). Fieldnotes were reviewed and each 15-minute block of observation time was assigned a primary activity code (e.g., idle time, medical procedure, physical therapy). Data were aggregated and analyzed using R statistical software. Code frequencies were used to calculate a patient “availability index” which illustrates times patients are most/least available (e.g., to potentially participate in Whole Health activities). In addition, we interviewed a subset of patients to understand their views on Whole Health. Interviews were conducted over the telephone, recorded, and transcribed. Content analysis was conducted on interview transcripts.
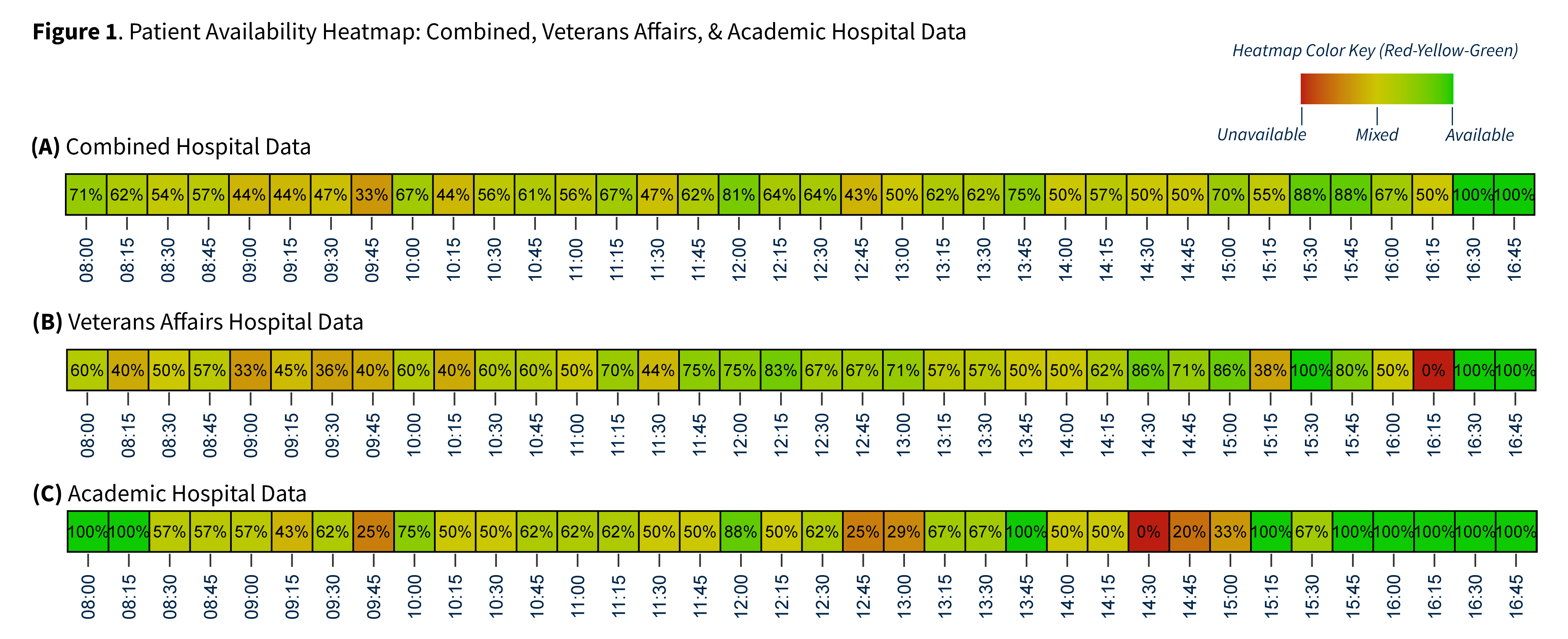
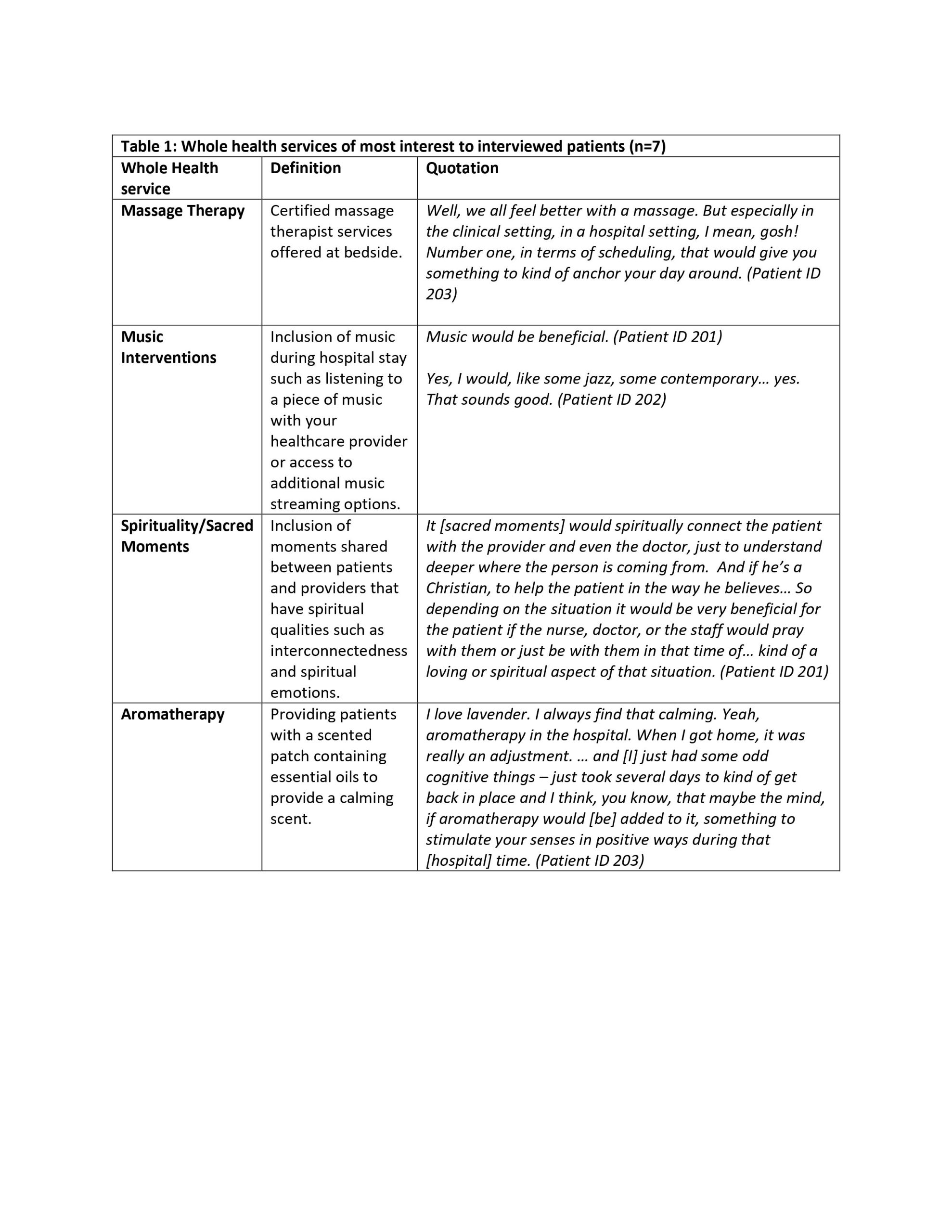
Results: A total of 11 patients at both hospitals were observed over 115 hours, and 7 patients were interviewed. From the availability index, we identified times when patients may be available to participate in Whole Health activities. Patients were most available between 3:00 and 5:00 PM and generally unavailable in the mornings between 8:30 and 11:00 AM. There were some differences between hospitals regarding when patients were most available (Figure 1). A total of 462 coded blocks were included in the availability index. Idle time (e.g., time when patients were alone watching TV, using their phone/tablet, daydreaming) was by far the most frequently coded activity (n = 137). Other frequently coded activities included clinical interactions (n = 63), time sleeping (n = 61), and time undergoing medical procedures (n = 43). Interview findings showed that all seven patients reported that they would be interested in participating in Whole Health activities during a hospital stay. In particular, patients were most interested in inclusion of massage therapy, music interventions, spirituality/sacred moments, and aromatherapy (Table 1).
Conclusions: Findings from our patient journeys revealed that patients had substantial idle time during hospital stays, particularly during the mid to late afternoon, when they could potentially participate in Whole Health activities. Importantly, interviewed patients reported being interested in these services and felt they could potentially provide benefit.