Background: Interprofessional collaboration (IPC) is vital for high-quality patient care, and effective IPC among medical professionals, especially trainees, is crucial to supporting positive individual and team outcomes. Measuring IPC and understanding its impact on patient care remains underexplored. Understanding which IPC patterns are associated with better patient and individual outcomes will inform how to best educate our medical professionals and ensure high-quality IPC.
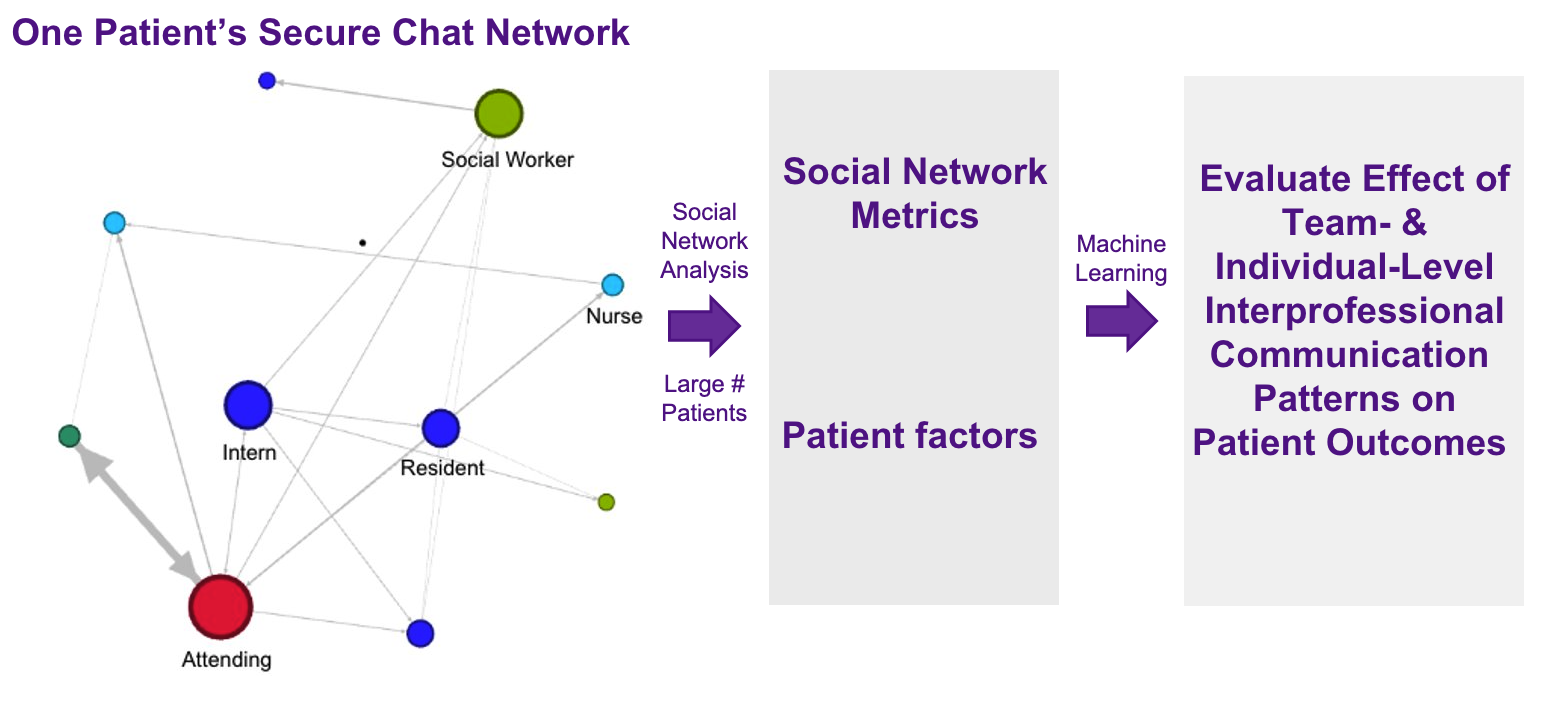
Methods: This cross-sectional analysis included data from 1,026 inpatient heart failure hospitalizations at NYU Langone Health from 2021 and 2023 and associated metadata derived from secure messages sent using Epic Secure Chat. Our dependent variable is observed-to-expected length of stay (O:E LOS) and we included over 100 independent variables from categories such as patient factors (i.e., comorbidities), and both hospitalization-level social network analysis metrics (i.e., density and reciprocity) and individual-level metrics (i.e., average medicine intern betweenness centrality). We utilized two machine learning models (ordinary least squares regression – OLS – and explainable boosted machine – EBM) to analyze and identify IPC features that describe patients’ O:E LOS variance when controlling for other important variables as mentioned above.
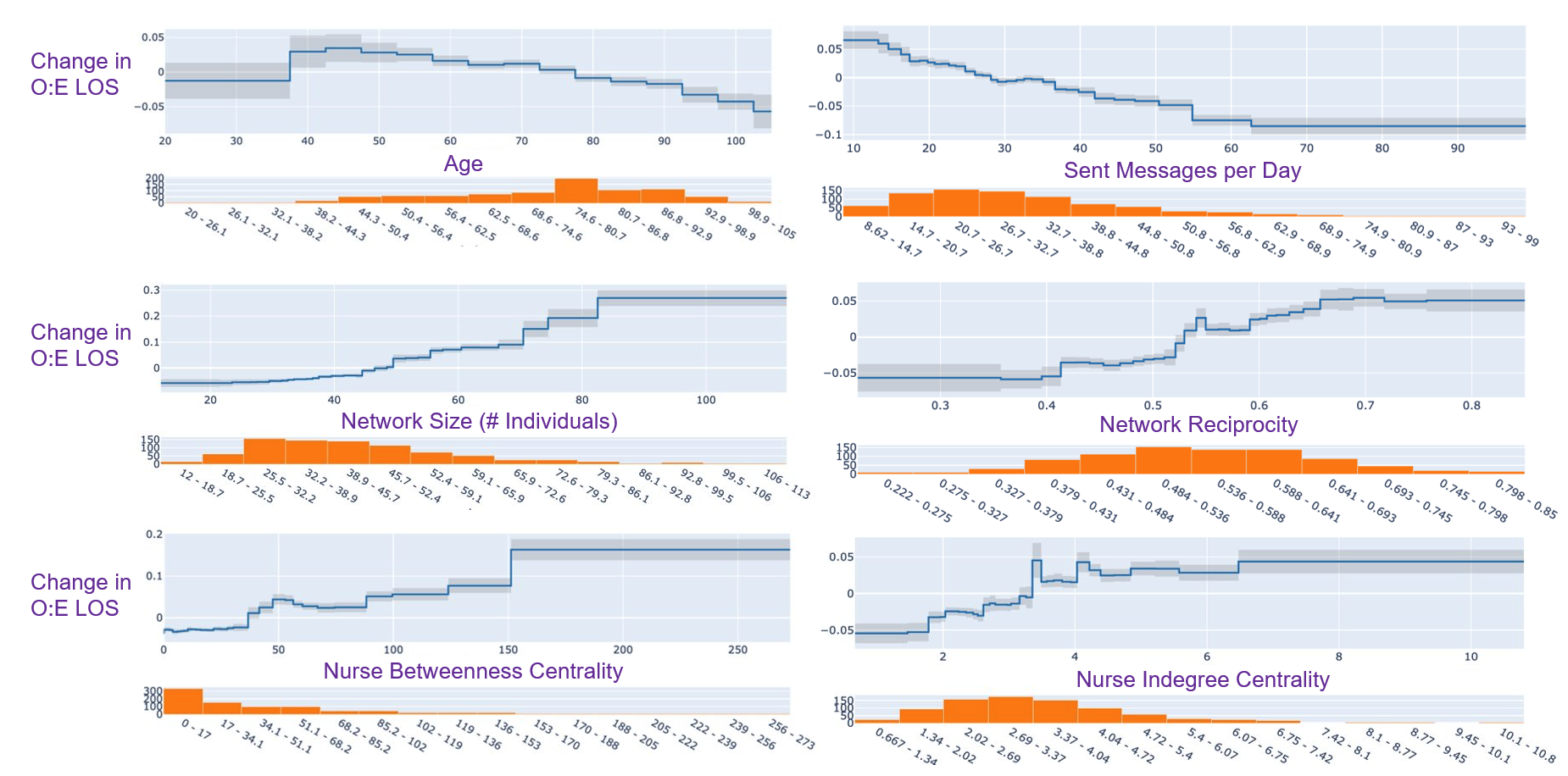
Results: Both models performed comparably (mean squared error was 0.10 and 0.14 for the OLS and EBM models, respectively) and identified variables derived from IPC that were important to explaining O:E LOS variance. With OLS, certain IPC-related features were associated with increased O:E LOS, such as network reciprocity and nurse indegree centrality, while others such as sent messages per day and social worker/care manager transitivity were associated with decreased O:E LOS. With EBM, we identified 14 important variables related to IPC (e.g., network density, nurse betweenness centrality, sent messages per day) that contributed significantly to variance in O:E LOS and could be explored further in graphical format.
Conclusions: EHR data of IPC among medical professionals explains a significant amount of variance in heart failure inpatients’ O:E LOS, when controlling for patient factors. This initial step leveraging EHR data to examine IPC using advanced data analytics has identified targeted areas for future interventions that can inform IPC best practices and ultimately enhance patient care.