Background: Adverse events (AEs) occur in 19-28% of hospitalized patients in the 30 days after discharge [1,2]. Though new or worsening symptoms (NWS) reported by patients are often an early indicator of post-discharge AEs, they are not systematically captured in electronic health record (EHR) documentation or via patient portals. Higher fidelity capture of patient-reported NWS during care transitions could lead to earlier detection of potential AEs. The purpose of this study was to characterize the type and frequency of patient-reported NWS, and their association with post-discharge AEs.
Methods: We performed a secondary analysis of a cohort of 260 patients discharged from a 171-bed academically-affiliated community hospital in Boston, MA between 9/2018 and 3/2020. All patients were offered a 30-day post-discharge phone call. All cases previously underwent manual chart review by 2 clinician reviewers trained to independently identify NWS and assess AEs based on objective EHR documentation [2]. Reviewers also identified patient-reported NWS, defined as subjective symptoms reported in home care visits, patient messages, or phone calls available in the EHR, or during a 30-day follow-up call regardless of objective clinician documentation. We performed a univariate analysis of each patient-reported and clinician-documented NWS and AEs. Next, we defined high-risk patient-reported NWS as those with the largest odds ratio (OR) which were consistent with clinician-documented NWS. Finally, we also performed a univariate analysis of high-risk patient-reported NWS and AEs.
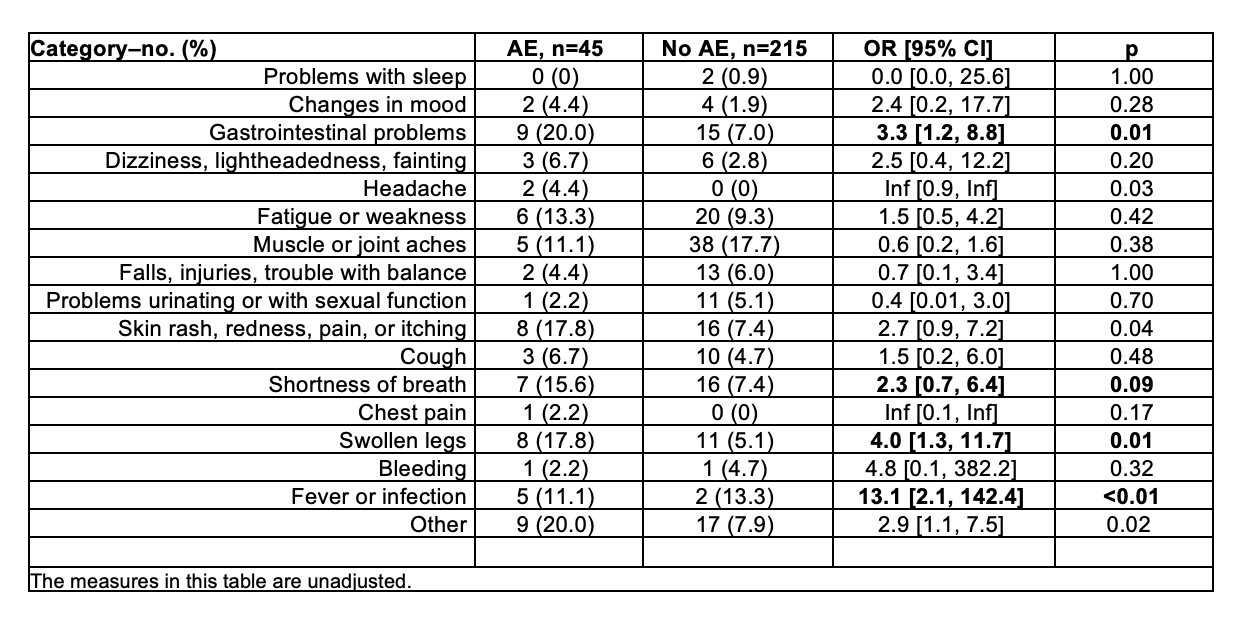
Results: Of 260 patients (mean age 62.5 years, 56% female, 63% Caucasian, 96% English speakers), 150 (57.6%) completed the 30-day phone calls. Six patient-reported NWS were independently associated with AEs (Table 1). Clinician-documented NWS associated with AE’s were similar (Table 2). The high-risk patient-reported NWS were gastrointestinal problems (2.3 [1.1, 4.8], p = 0.02), shortness of breath (3.0 [1.3, 6.7), p = 0.01), swollen legs (5.1 [1.7, 15.0], p < 0.01), and fever/infection (5.5 [1.7, 18.1], p < 0.01). Collectively, high-risk patient-reported NWS (3.76 [1.89, 7.82], p< 0.01)) were strongly associated with AEs.
Conclusions: In this secondary analysis, we observed that certain high-risk patient-reported symptoms were commonly associated with post-discharge AEs, and were similar to clinician-documented NWS. While these results require further validation, remote symptom monitoring and care management interventions that consider specific types of patient-reported symptoms could lead to earlier detection of AEs during care transitions.