Background: Patient safety assistants (PSAs), or “sitters,” observe patients at bedside considered at “high risk” for in-hospital events [1] such as falls or elopements. While studies suggest PSAs do not impact safety outcomes,[2-4] they are widely utilized without formal guidelines.[2, 5, 6] With increasing healthcare costs and limited resources, efficient care models are sought.[1, 2, 7] Accordingly, this quality improvement (QI) project aimed to evaluate the effect of a nurse driven sitter protocol on PSA utilization and patient safety at a large publicly funded county hospital.
Methods: A nurse driven sitter protocol was implemented at a large, public, academic safety-net hospital to decrease unnecessary PSA use. PSAs utilized for involuntary holds and suicide precautions were excluded. Sitters were previously ordered by physicians and advanced practice providers (APPs) for patients felt to present a safety risk to themselves, particularly those with altered mental status (AMS). This nurse driven protocol empowers nursing to order and discontinue sitters without physician approval and requires a more detailed categorization of sitter indication: pulling lines/drains/tubes, fall risk, ingesting foreign objects, wandering/climbing, AMS. The protocol was implemented hospital-wide on March 1, 2019. A random sample of 60 patients requiring sitters from December 1, 2018 to February 28, 2019 was compared to a random sample of 62 patients from March 1, 2019 to May 31, 2019. Safety of the intervention was measured by comparing patient falls per sitter day, rapid assessment team (RAT) calls, behavioral emergency response team (BERT) evaluations and patients leaving prior to treatment completion (LBTC). Two-sided t-tests and Mann-Wilcoxon tests were used to compare continuous variables. Chi-square tests were used to compare categorical variables. SAS version 9.4 was used for all analyses. P-values of <0.05 were considered significant.
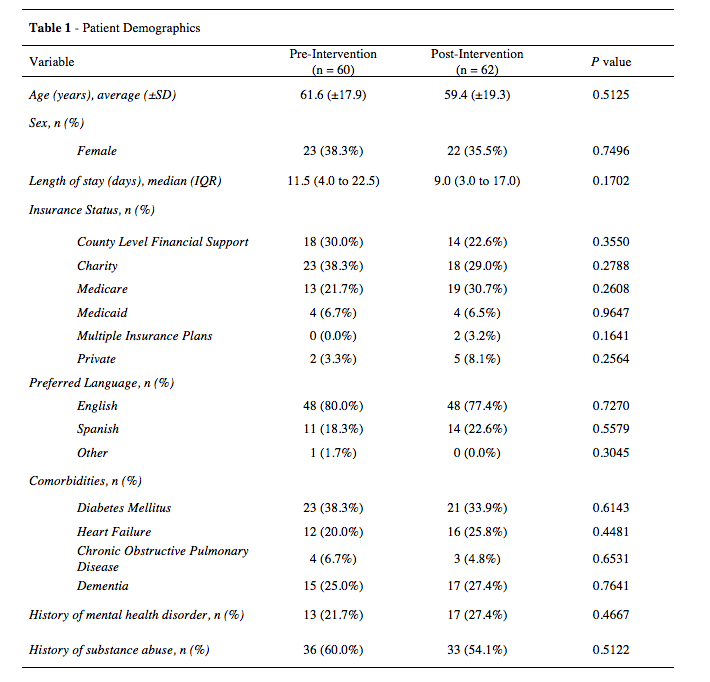
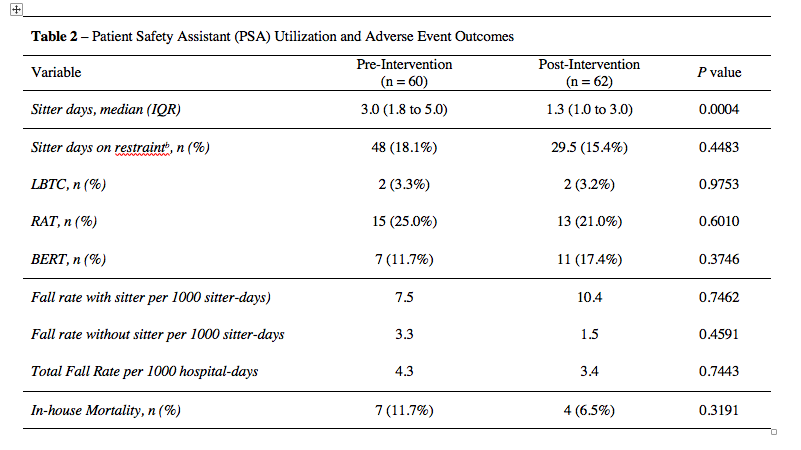
Results: There were no significant differences in baseline characteristic of the patients pre and post intervention (Table 1). The median sitter utilization was 3.0 days (IQR 1.8 – 5.0) pre-intervention and 1.3 days (IQR 1.0 – 3.0) post-intervention (p<0.001). There was no change in number of patients who LBTC: 2 (3.3%) pre-intervention vs. 2 (3.2%) post-intervention (p=0.98). There was no difference in RAT evaluations: 15 (25.0%) pre-intervention vs. 13 (21.0%) post-intervention (p=0.60), BERT evaluations: 7 (11.7%) pre-intervention vs. 11 (17.4%) post-intervention (p=0.37), or falls per 1000 hospital days (4.3 vs 3.4; p=0.74).
Conclusions: This QI initiative suggests that a nurse driven protocol for PSA utilization is both effective and safe without resultant increases in falls or other safety events. The safe reduction in sitter utilization in a resource constrained safety net hospital allows for reallocation of PSAs to the work of patient care assistants, helping to offload nursing staff which may also improve overall safety as well as nursing satisfaction. Decreased time spent as a sitter may also improve PSA staff satisfaction. Additionally, this nurse drive sitter protocol decreases physician and APP workload which may further leverage organizational resources while improving wellness and retention.