Background: The Agency for Healthcare Research and Quality recommends a structured, patient-centered discharge communication process. To create patient-centered discharge communication, it is vital to understand the information that patients value upon discharge. Little is known about how patients prioritize discharge information; therefore, our objective was to determine the perceptions of hospitalized patients about the relative importance of discharge communication elements.
Methods: We conducted a survey of patients admitted on the hospital medicine service using a tool that included the following 6 discharge information elements: discharge medications, hospital stay summary, discharge instructions, dietary/activity restrictions, when to call 911/doctor, and follow-up information. Patients were asked to rank each element from 1 to 7 (the most important to least important) using each ranking once. Age, gender, race, education level, number of medications, and comorbid conditions were self-reported by patients. We excluded patients who did not provide consent or were unable to complete the survey due to language or physical barriers. To account for the complex ordered ranking, we used Plackett-Luce model to determine relative ‘worth’ of each element to the patients. To examine if patient characteristics affect a given item’s ranking, we used Kruskal-Wallis rank test; for ranking patterns we used multilevel ordered logistic models.
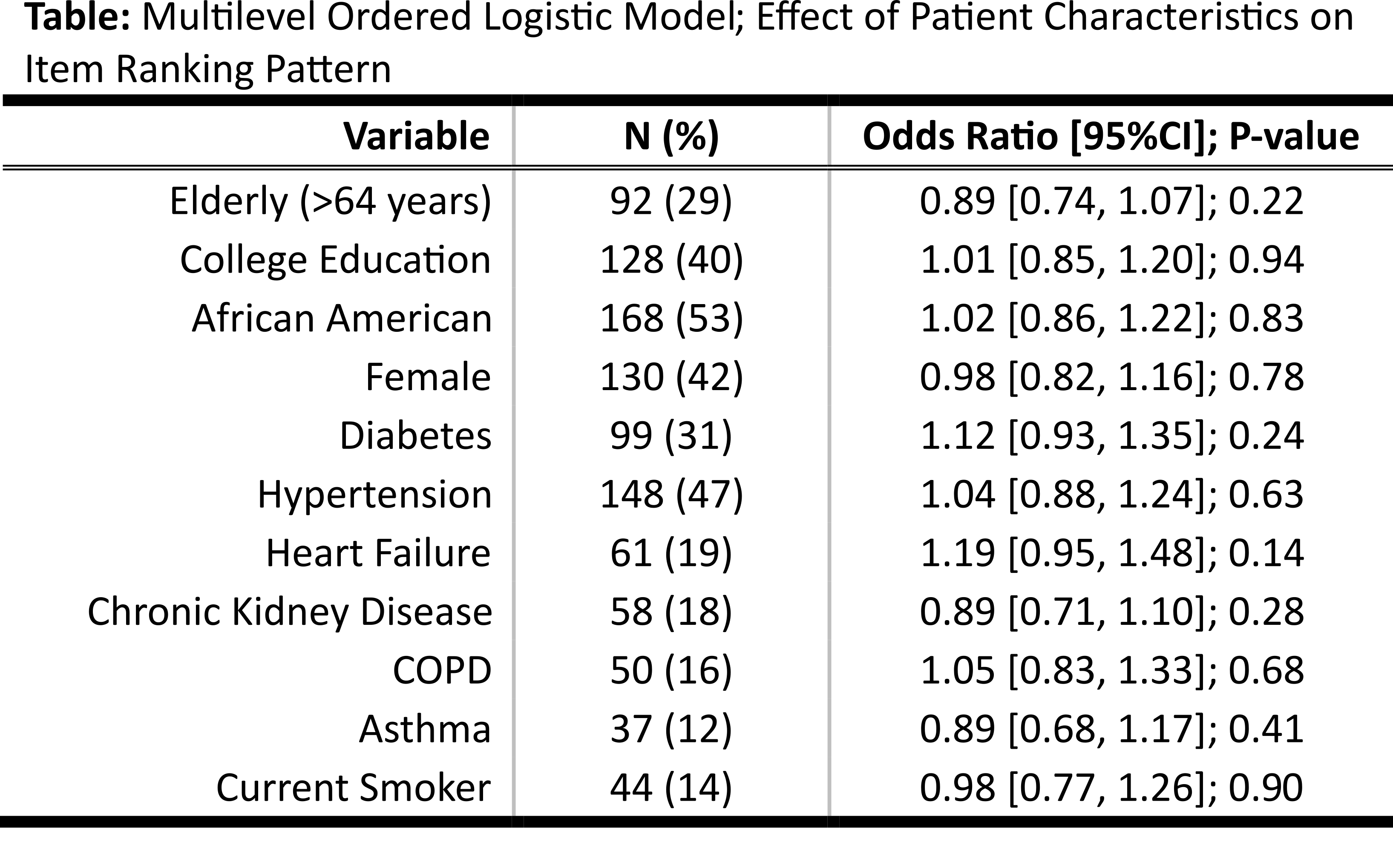
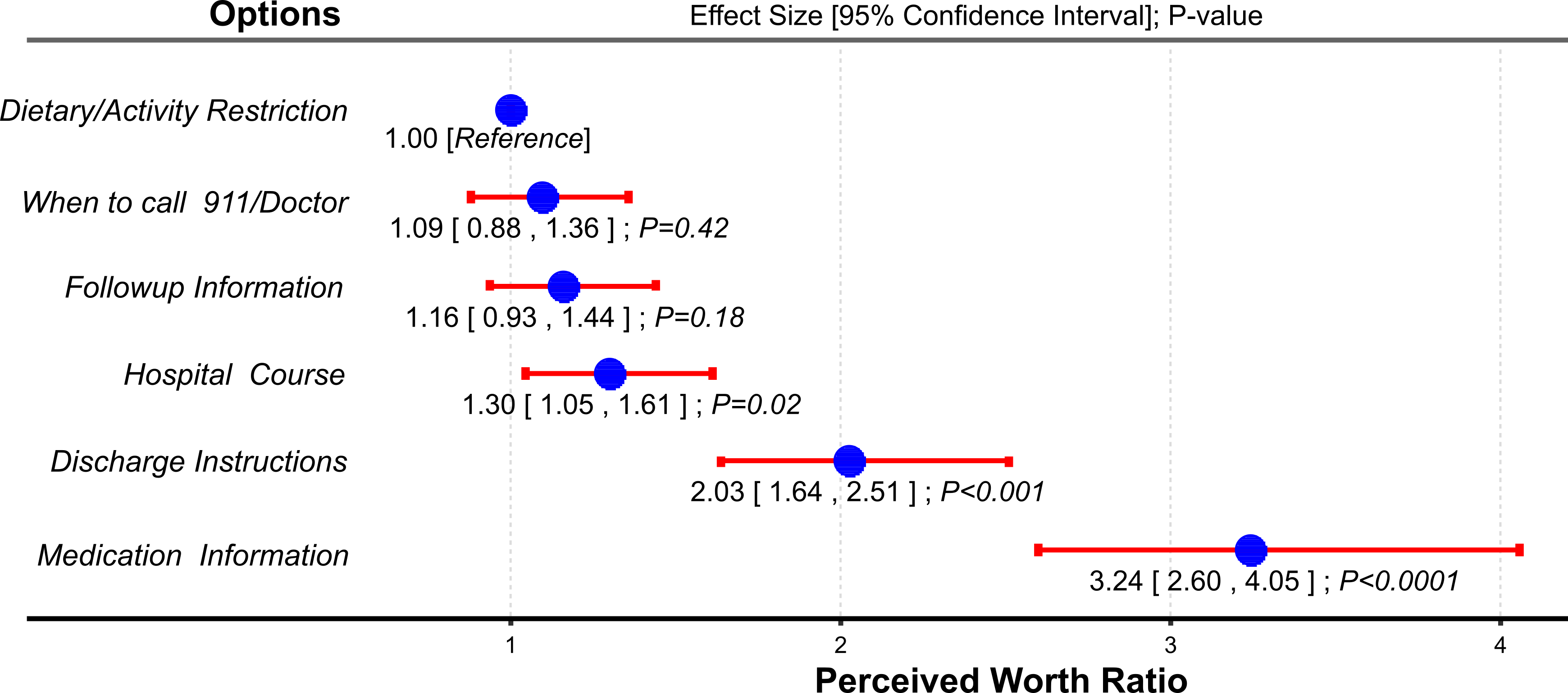
Results: Of the 317 surveyed patients, 179(60%) were males with a mean(SD) age of 56(13) years. The relative worth for patients of discharge medication information was 3 times greater than the dietary/activity restrictions (worth ratio: 3.24; P<0.001). While discharge instructions and hospital course summary also had greater worth than dietary/activity restrictions, follow-up information and when to call 911/doctor had similar worth (Figure). We found statistically significant differences in individual item ranking by participant characteristics; African Americans, heart failure patients, and individuals without college degree ranked information on when to call 911/doctor higher than others (P-value=0.05, 0.04, 0.001 respectively). However, in multilevel ordered logistic models, we did not find any association between ranking and population characteristics (Table).
Conclusions: Hospitalized patients rated information on medications as the most important discharge communication. Whether committing resources to communicate discharge elements based on patient’s perceived importance results in better health outcomes needs to be seen.