Background: Excellent onboarding processes can promote employee engagement, satisfaction and retention (1), yet there is minimal research about optimal practices for onboarding hospitalists (2). With potential PHM workforce challenges looming, it is essential to understand the current landscape of onboarding in PHM.
Methods: We surveyed leaders of PHM groups about their onboarding practices. The survey, developed with expert input from group leaders, included multiple choice questions and free-text responses to elicit descriptions of PHM leaders’ current onboarding practices and their perception of the quality and efficacy of their onboarding. The survey was distributed via the AAP Section of Hospital Medicine Division Leaders listserv.
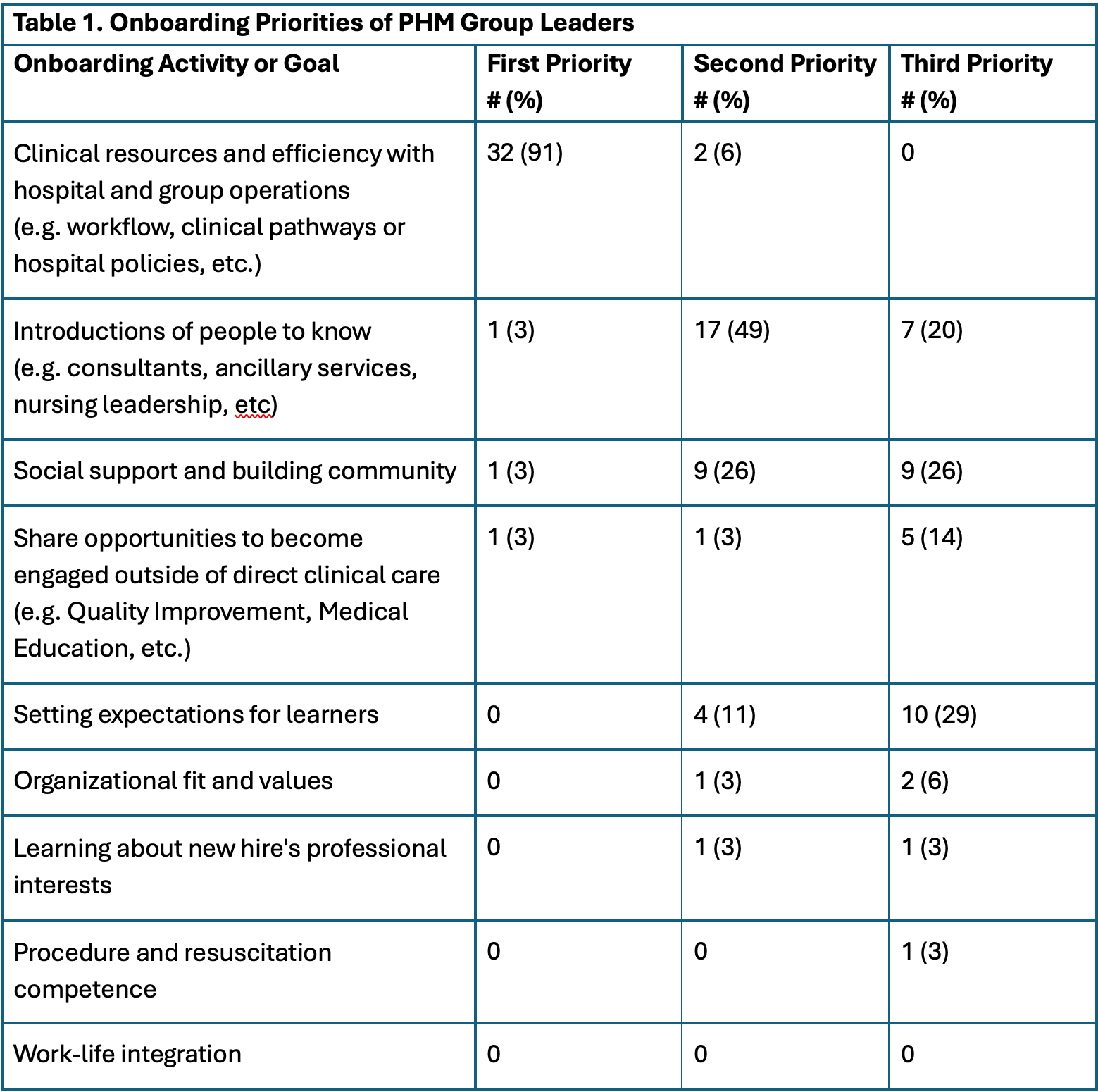
Results: Thirty-five discrete sites completed the survey, and two other sites responded indicating no formal onboarding processes. Respondents worked at a variety of hospitals including freestanding, free-leaning children’s hospitals, and community hospitals. Nearly all respondents felt their onboarding processes were at least somewhat effective, with twelve (34%) describing their onboarding as “very effective” and two (6%) designating their onboarding as “extremely effective.” The two respondents who considered their onboarding “extremely effective” described on-the-job orientation as their top strength, requiring new hires to shadow before their first shift and scheduling new hires to work with “an experienced hospitalist” for their first shifts, thereby allowing “lots of opportunities to see how things work and ask questions” while providing patient care.PHM group leaders were fairly consistent regarding top priorities (Table 1). Nearly all indicated their top priority was orienting new hires to hospital resources for efficiency in their clinical care. “Setting expectations for learners” was the second priority for almost half of respondents. Other top priorities included: social support and community building, introducing people to know, and sharing opportunities to become engaged outside of direct clinical care. Fewer than 10% of respondents selected the following priorities: learning about new hire’s professional interests, organizational fit, procedure resuscitation competence. Interestingly, no one chose work-life integration as one of their top three onboarding priorities.There was a wide range of onboarding activities: all groups included shadowing, numerous respondents emphasized the value of shadowing and pairing new hires with experienced hospitalists for their first shifts; nearly all provided a written onboarding guide. Some groups required activities such as procedure simulation and orientation meetings with designated hospital leaders.
Conclusions: Our results are reassuring that PHM groups have formal onboarding practices and group leaders are satisfied with their efficacy. Despite this, there seem to be opportunities for improvement in onboarding, which is essential to increasing retention and employee satisfaction. Shadowing and opportunities to collaborate with staff familiar with the hospital were highly prioritized by group leaders, and their onboarding also emphasized how new hires should teach learners. These results offer ideas for the implementation of onboarding processes, while underscoring the need to assess the perspectives of the employees to have a broader picture of best practices.