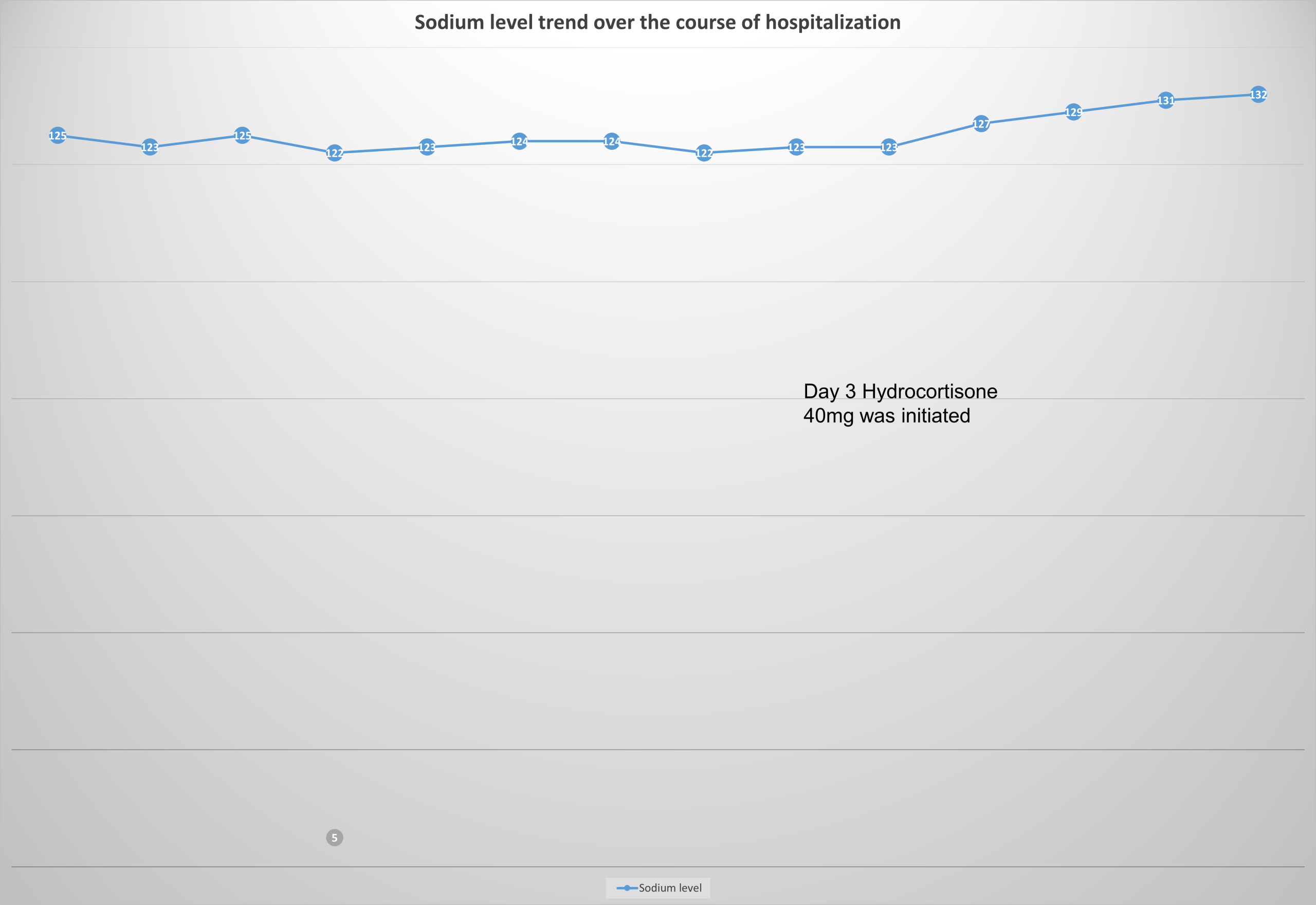
Case Presentation: 75-year-old female with a past medical history of triple negative breast cancer, Stage IIB, undergoing adjuvant radiation therapy, on cycle 3 of pembrolizumab, presented with fatigue and myalgia. On Day 1, she was found to have hyponatremia with a sodium level of 125 mmol/L, urine osmolality of 227 mOsm/kg, and urine sodium of 31 mmol/L. Due to her history of poor oral intake, she received a 1 L normal saline (NS) bolus and was started on maintenance fluids for suspected hypovolemic hyponatremia. However, a repeat sodium check showed a worsening level at 123 mmol/L. Intravenous fluids were subsequently discontinued, and the patient was started on sodium chloride tablets (1 g). Two subsequent readings showed an improvement in her serum sodium levels (125 mmol/L and 128 mmol/L, respectively). The sodium chloride tablets were discontinued after two doses on Day 2. However, after discontinuation, her serum sodium levels, which were checked every four hours, continued to trend downward over Days 2 and 3 (125 mmol/L → 122 mmol/L → 123 mmol/L → 124 mmol/L → 124 mmol/L → 122 mmol/L → 123 mmol/L). On Day 3, repeat urine osmolality was 293 mOsm/kg, and urine sodium was 80 mmol/L. Further workup revealed a low serum cortisol level of 3.3 mcg/dL. ACTH stimulation test (250 mcg) showed low serum cortisol levels at 30 and 60 minutes (4.9 mcg/dL and 6.6 mcg/dL, respectively). Serum ACTH was within the lower half of the reference range (14 pg/mL). The patient was diagnosed with central adrenal insufficiency secondary to pembrolizumab and was started on hydrocortisone 40 mg twice daily. By discharge on Day 5, her serum sodium was 132 mmol/L, and her symptoms of fatigue and myalgia had resolved.
Discussion: Pembrolizumab, an immune checkpoint inhibitor (ICI), is a monoclonal antibody that blocks the programmed death receptor-1 (PD-1)/programmed death ligand 1 (PD-L1) pathway. ICIs, while effective, can lead to immune-related adverse events (irAEs), the most common being hypothyroidism. Hypophysitis, a rare irAE caused by anti-PD-1 antibodies, occurs in less than 1% of patients. Hypophysitis associated with ICIs can result in secondary adrenal insufficiency (AI) and hypopituitarism. Given that hypophysitis can be life-threatening if not promptly treated, early detection and steroid initiation are essential. Some hyponatremic patients who appear euvolemic may initially present with low urine sodium and high urine osmolality, like this patient. In these cases, repeating urine sodium and urine osmolality after the infusion of NS can help clarify the diagnosis. If the hyponatremia is due to hypovolemia, NS will reverse the stimulus for antidiuretic hormone (ADH) secretion, promoting water excretion and leading to a rapid correction of serum sodium levels. Conversely, if the hyponatremia is caused by hypocortisolism (cortisol deficiency causes increased vasopressin secretion), NS may exacerbate the condition and further lower serum sodium. In these patients, urine sodium levels will increase as hypovolemia is corrected, while urine osmolality remains elevated, like seen in our patient.
Conclusions: Although rare, AI should be considered in patients receiving ICIs, when presenting with symptoms of fatigue, hyponatremia, hypoglycemia, hyperkalemia, and hypotension. Endocrine function tests, including cortisol and ACTH levels, are essential for diagnosis. Despite the increasing reports of secondary AI associated with ICI treatment, it remains an uncommon occurrence.