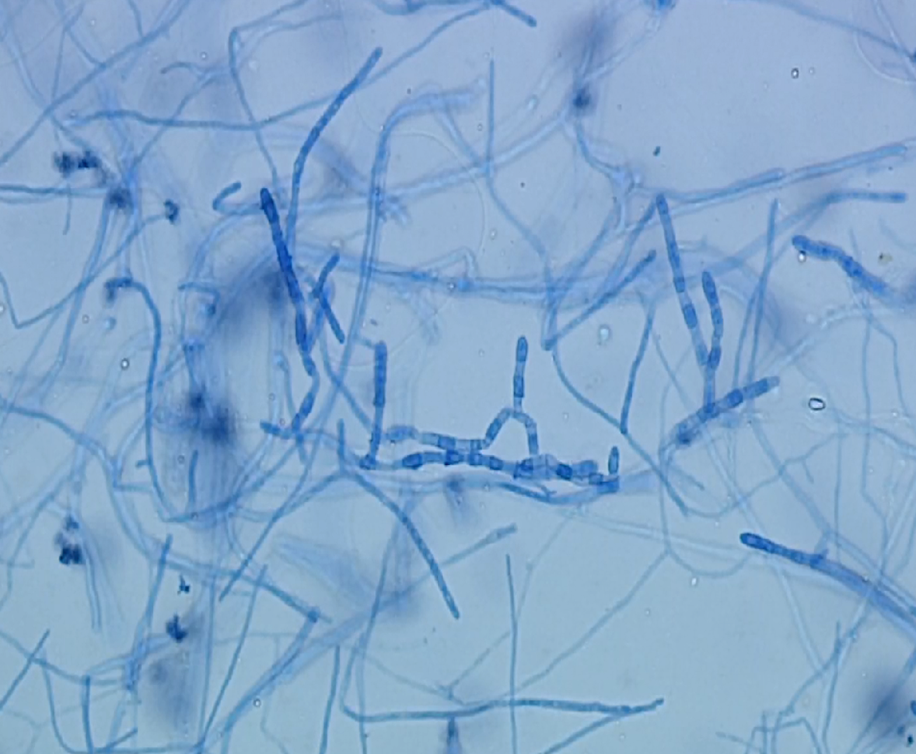
Case Presentation: A 50-year-old Filipino man with poorly controlled type 2 diabetes mellitus presented with 4 days of fever, abdominal pain and distention. He endorsed unintentional weight loss of 30lbs over the last year as well as a chronic cough. The physical exam was notable for bibasilar lung crackles and abdominal distention with diffuse tenderness to palpation and rebound. Labs revealed a white blood cell count of 9.9K/μL with an absolute eosinophil count (AEC) of 1.7 K/μL (17.4%). A chest x-ray showed a left lower lobe lung consolidation. Abdominal CT demonstrated large ascites without cirrhosis and innumerable nodules studding the omentum. Ascitic fluid contained >6,000 leukocytes (53% neutrophils, 30% lymphocytes, 10% macrophages, 5% eosinophils). Fluid cytology was negative for malignancy. Peritoneal and sputum studies for tuberculosis returned negative. Serologies for Cryptococcus, Strongyloides, HIV and Hepatitis C were also negative. Coccidioides serologies returned positive for IgG and IgM antibodies with a complement fixation titer of 1:2. Ascitic fluid grew white mold identified as Coccidioides immitis. The patient was discharged on Fluconazole 400 mg PO daily for 12 months.
Discussion: Less than 1% of coccidioidomycosis (CM) cases disseminate following an initial pulmonary infection. Systems most commonly affected include skin, bone, and meninges. Previous cases describing peritoneal involvement are rare, ranging from an asymptomatic inguinal mass to acute peritonitis. Previously proposed mechanisms of pathogenesis in intra-abdominal coccidioidomycosis (IAC) include either hematogenous spread from a primary lung infection or ingestion of pulmonary secretions. Manifestations of abdominal infection can occur weeks to years following initial pulmonary infection. This time course appears consistent with our patient’s unintentional weight loss and cough over the preceding year.
Our patient’s initial presentation was highly concerning for malignancy. While IAC can mimic peritoneal carcinomatosis, to our knowledge, this is the first reported case of a patient with ascites and omental nodularity where peripheral eosinophilia provided an important diagnostic clue for the presence of disseminated Coccidioides.
Conclusions: Our case highlights a unique triad of clinical findings: peritonitis, omental nodularity, and peripheral eosinophilia, that led to a diagnosis of IAC. Clinicians should be aware of this atypical presentation and triad of findings, particularly in endemic areas, in order to avoid misdiagnosis.
.jpg)
