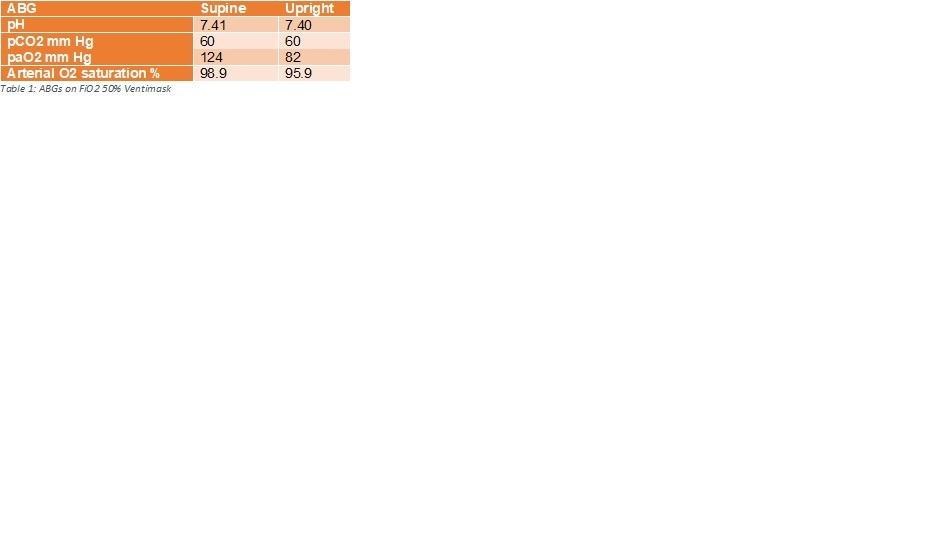
Case Presentation: We describe a case of a 76 year old male with history of advanced centrilobular emphysema who developed platypnea and orthodeoxia. He was diagnosed with severe obstructive disease since 4 years and was on home oxygen. He had multiple admissions for dyspnea with treatment including supplemental oxygen, bronchodilators, steroids and antibiotics. His oxygen saturation was 94% on 4 litres oxygen when lying down. However, on standing, his oxygen saturation decreased to 84% on the same amount of oxygen. Finger pulse oximetry at bedside was repeated with positional variation. The following pulse oximetry readings were recorded on 8 L of supplemental oxygen – 92-94% supine, 88-89% sitting up, 86-88% standing up and 93% on supine again. ABGs were drawn on 50% FiO2 via Venti mask in supine and upright positions with 11 minutes equilibrium time in between. The A-a gradient increased from 157.50 mm Hg in supine to 199.5 mm Hg in upright position. Transthoracic echocardiogram showing no evidence of right to left intracardiac shunt in the upright position. CT angiogram was negative for vascular malformation or pulmonary arterial shadow suggestive of an arteriovenous shunt.
Discussion: Platypnea is defined as dyspnea induced by upright posture and relieved by recumbence. Orthodeoxia is arterial oxygen desaturation in a similar setting. The first case was reported in 1949 and the most common etiology is either anatomic or functional right to left interatrial shunt. These include patent foramen ovale, atrial septal defect or atrial septal aneurysm. Platypnea and orthodenoxia syndrome (POS) has been rarely associated in case reports with pulmonary causes. These include advanced emphysema, amiodarone toxicity, post-pneumonectomy state, ARDS and recurrent pulmonary embolism. We describe one such rare case of POS in advanced emphysema without evidence of other etiologies. Normal physiology dictates that apex of the lung receives lower perfusion in upright position due to lower capillary pressure. In patients with emphysema, the alveolar pressure is higher than normal leading to less perfusion. Additionally, sitting upright further reduces perfusion in lung apex increasing dead space.
Conclusions: Advanced progressive pulmonary disease should be recognized as a possible etiology for POS in patients with no interatrial shunts. Our recommendation for the patient included higher flow oxygen delivered through a home oxygen concentrator when sitting or walking upright. Further treatments options need to be explored to reduce symptoms in such patients.