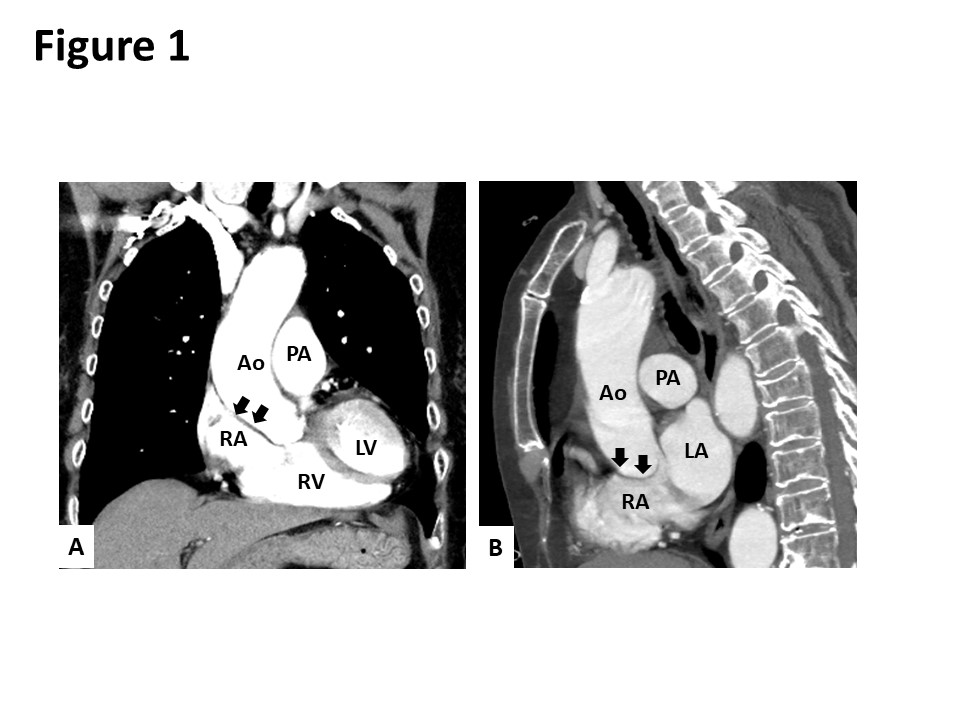
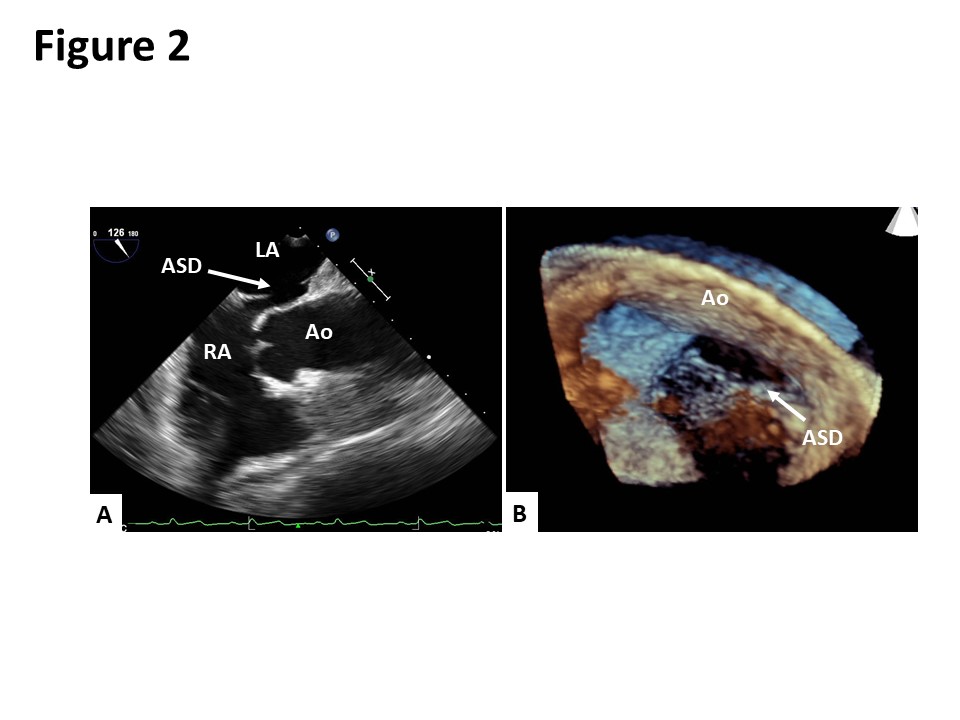
Case Presentation: An 80-year-old Japanese woman presented to our hospital with dyspnea in the sitting and standing positions. Two months prior to her admission, she had presented to another hospital with multiple vertebral compression fractures. After being discharged from the hospital, she developed dyspnea in the sitting and standing positions. She also reported an episode of syncope. Although the patient’s oxygen saturation on room air was 98% in the supine position, it declined to 83% in the sitting position and dropped further to 65% in the standing position. Contrast-enhanced computed tomography revealed the elongation of the aorta, which was compressing the right atrium and distorting the position of her heart (Figure 1). A transesophageal echocardiogram showed an oval-shaped secundum atrial septal defect (ASD) measuring 14 mm x 7 mm in size with a deficient aortic rim (Figure 2). The surgical closure of the ASD was performed. Following surgery, her oxygen saturation in the sitting and standing positions recovered to 98% on room air. She was discharged on the 23rd day after the surgery without any complaints of platypnea.
Discussion: Platypnea-orthodeoxia syndrome (POS) is a rare syndrome characterized by dyspnea and hypoxia when a patient is sitting or standing. The most common anatomical cause of POS is a right-to-left (RL) shunt through interatrial communications, including an atrial septal defect (ASD) or patent foramen ovale (PFO). In our case, based on the patient’s clinical course, her multiple vertebral compression fractures were suspected to have triggered the exacerbation of the RL shunting. To the best of our knowledge, only three cases of POS induced by vertebral fractures have been reported. A possible etiological mechanism to explain the induction of POS by vertebral fractures is as follows: the multiple vertebral compression fractures caused kyphosis and the subsequent distortion of the aorta resulting in right atrial compression and increased RL flow through the ASD.
Conclusions: Based on the fact that ASD or PFO is present in approximately 15-35% of the normal population, and that the incidence of vertebral compression fractures has been increasing in our aging society, POS should be considered among the differential diagnoses when a patient develops dyspnea following vertebral compression fracture. The careful assessment of the patient’s history and clinical condition are essential for the accurate diagnosis of this rare disorder.