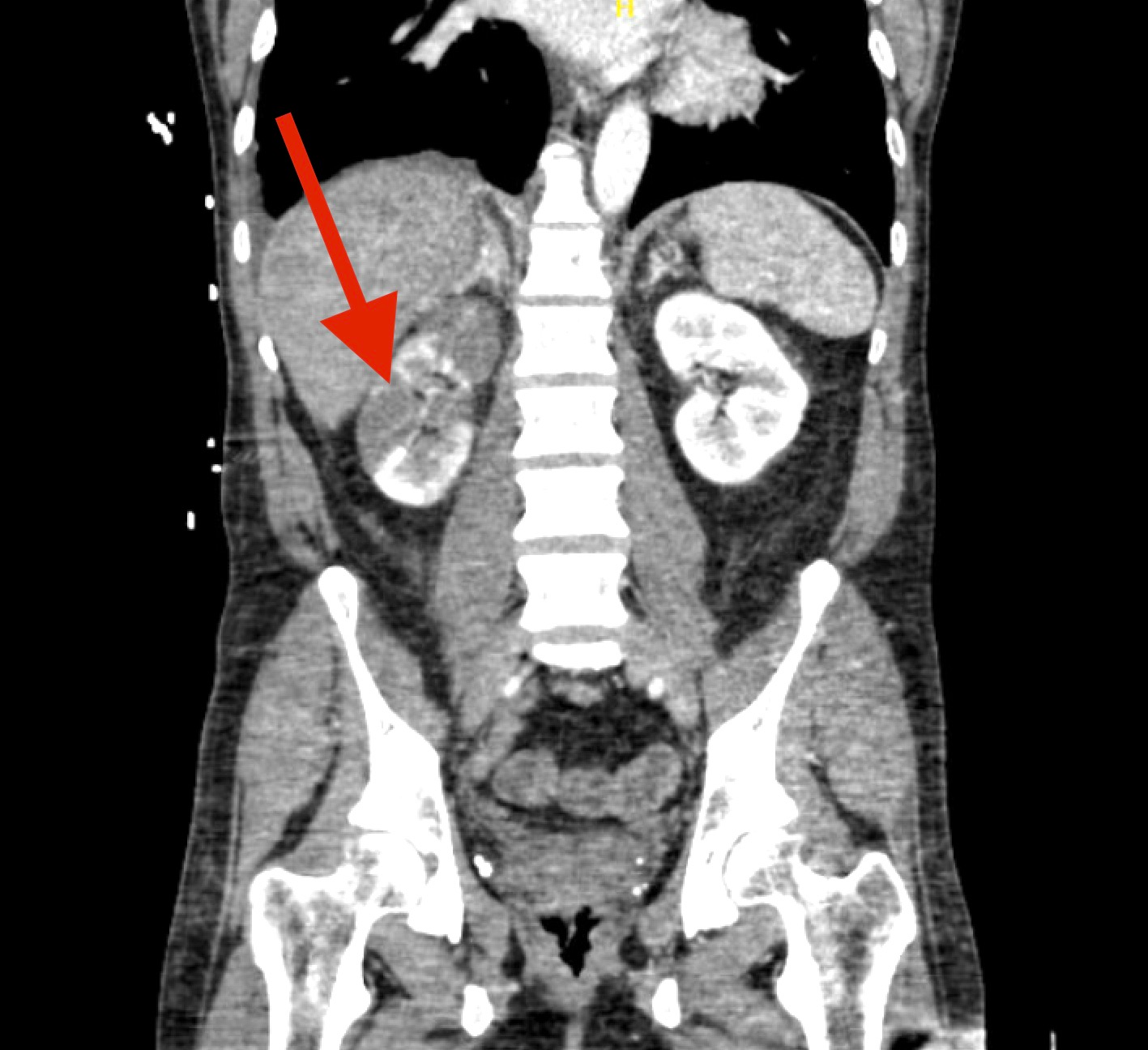
Case Presentation: A 41-year-old male with a past medical history of hypertension and occasional alcohol use presented to our facility for progressively worsening shortness of breath and flu-like symptoms of six days duration. The patient was started on oseltamivir at an urgent care two days prior to presentation. On evaluation, the patient was diaphoretic and appeared acutely ill. He was noted to be hypertensive and tachycardic. Blood work was significant for a leukocytosis of 15.5 x 0^3/mcL, creatinine 2.0 mg/dL, lactic acid of 4.3 mmol/L, and troponin T 218 ng/L. EKG on admission showed a left bundle branch block of indefinite duration. Shortly afterwards, the patient went into pulseless electrical activity requiring brief cardiopulmonary resuscitation. The patient achieved return of spontaneous circulation and was transferred to the ICU for vasopressor support and mechanical ventilation. Repeat EKG revealed ST segment elevation in lead V3. CT chest and abdomen demonstrated a left ventricular, internal vena cava, and iliac vein thrombus, as well as signs of systemic emboli with evidence of renal infarcts. Further evaluation of cardiac function with an echocardiogram showed an ejection fraction of 10% and severe left ventricular dysfunction. Anticoagulation with unfractionated heparin was commenced and the patient was taken for emergent cardiac catheterization with placement of an intra-aortic balloon pump. Coronary angiogram demonstrated nonobstructive disease. The patient was transferred to a tertiary care facility for consideration of veno-arterial extracorporeal membrane oxygenation. Over the next few days, he received supportive care for suspected viral myocarditis and showed remarkable improvement. The intra-aortic balloon was discontinued; he was successfully weaned from mechanical ventilation, and goal-directed medical therapy was initiated. The patient did not require hemodialysis and had no neurological deficits secondary to systemic emboli.
Discussion: Influenza virus, a common and highly infectious respiratory pathogen, has been associated with life-threatening myocarditis. The frequency of influenza-associated myocarditis has been reported up to 10%, with the prevalence being highest amongst young male adults. Viral myocarditis is caused by a release of pro-inflammatory cytokines leading to cardiomyocyte inflammation and endothelial cell dysfunction. The clinical spectrum can vastly vary from asymptomatic to fulminant myocarditis with concern for cardiogenic shock and cardiac arrest. Intraventricular thrombus is a known complication of acute viral myocarditis, however embolic insult to the kidney is a rare presentation. The treatment is mainly supportive, targeting viral infection and hemodynamic instability which significantly improves survival in such cases. Based on a national survey on fulminant viral myocarditis from Japan, 57.7% of patients who received hemodynamic support survived without receiving antiviral treatment, whereas the mortality associated with fulminant myocarditis was high without early mechanical circulatory support.
Conclusions: In conclusion, we report a case of a young male with symptoms of severe influenza and rapidly progressive fulminant myocarditis requiring an intra-aortic balloon pump. Our patient recovered from multi-organ failure with rapid pharmacological hemodynamic support and mechanical circulatory assistance.