Case Presentation: Exogenous lipoid pneumonia (ELP) is an unusual respiratory disease caused by inflammation from a foreign body reaction to inhaled lipid particles. Here we present a case of this illness in the absence of a history of vaping, and we show how diagnosis can be delayed while searching for more common respiratory disorders.
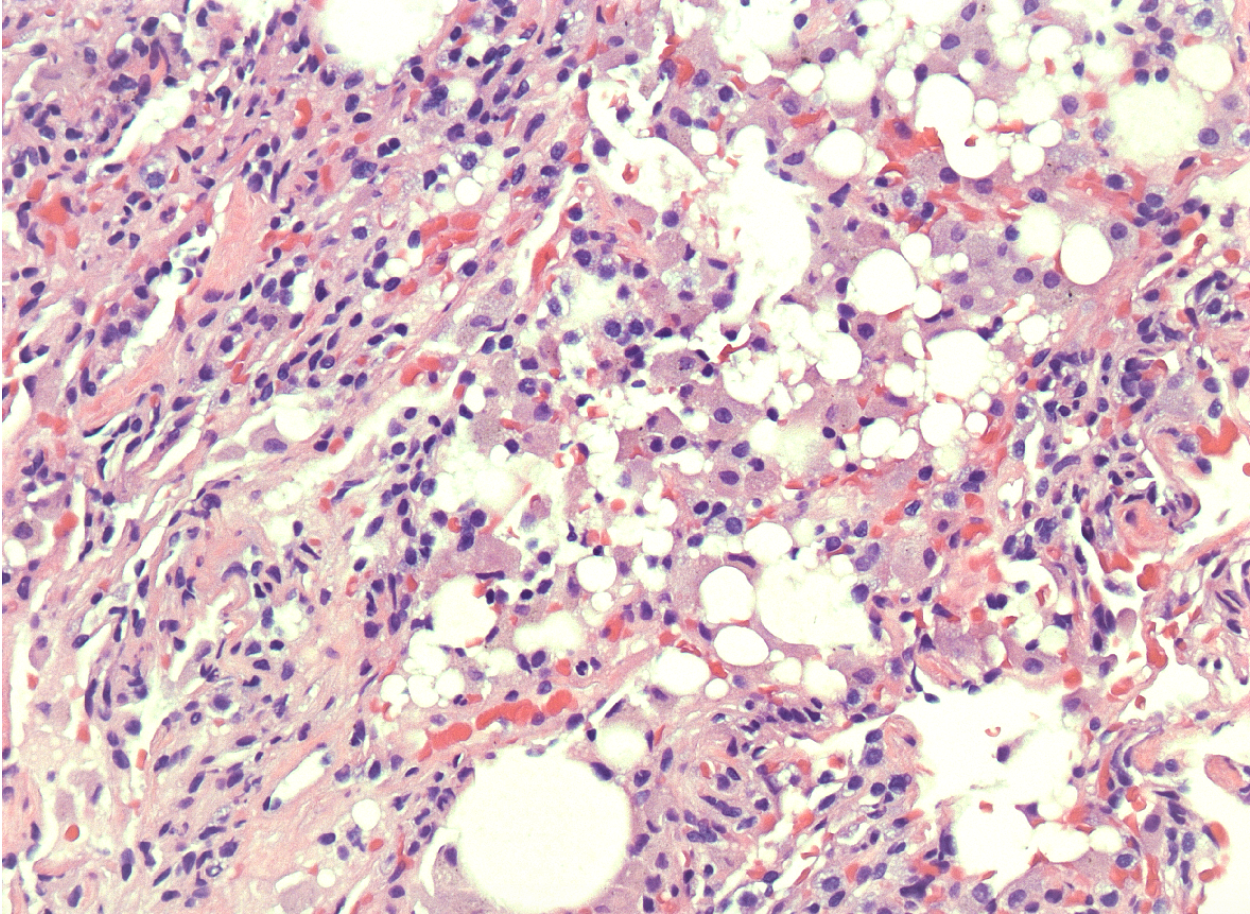
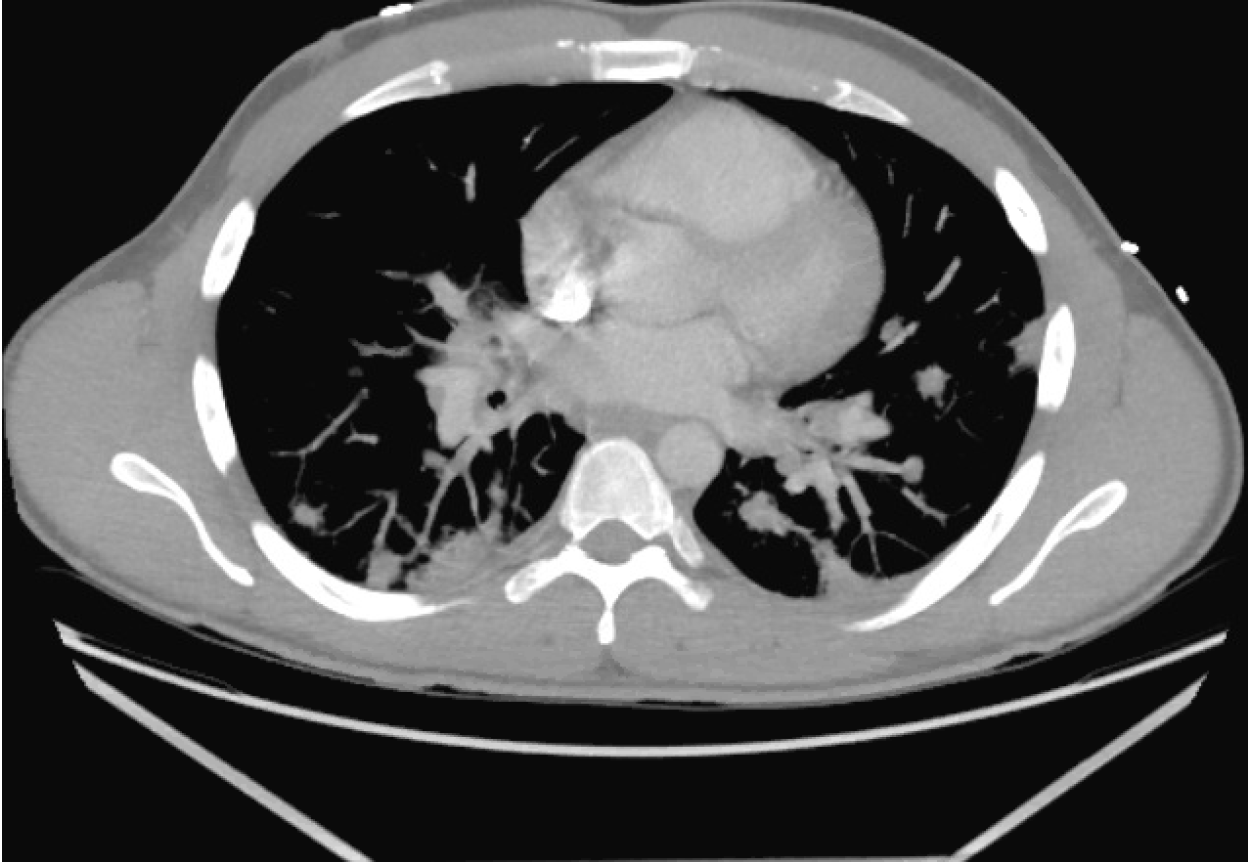
Discussion: A 27-year-old male presented to the emergency department with one week of shortness of breath, diaphoresis and body aches. His symptoms began after a recent trip to Florida, during which he reports lobster hunting. No one else on the trip felt ill. His symptoms started with intermittent diarrhea, reduced appetite, and mild diffuse abdominal pain and progressed over several days to include a productive cough, shortness of breath worse on exertion, and fevers peaking at 102.3 °F. The patient lives in a rural setting in Texas and works as a landscaper, using pesticides and fertilizers. He was in a year-long monogamous relationship without a history of sexually-transmitted diseases. He denied smoking, vaping and drug use, but drank alcohol socially. On admission, white blood cell count (10.4 x 103/µL) and liver enzymes (ALT 62 IU/L) were mildly elevated, but the remainder of his labs were unremarkable. A CT chest demonstrated bilateral pulmonary nodules with hilar and mediastinal lymphadenopathy, bilateral posterior lower lobe consolidations, and bilateral ground glass opacities (Image 1).The patient fevered nightly during the first 72 hours of admission despite broad spectrum antibiotics, and he complained of persistent, mild abdominal pain. His fevers finally resolved with scheduled acetaminophen on day 4. An extensive infectious workup was negative, and antibiotics were discontinued on day 5. Pulmonology performed a bronchoscopy, endoscopic ultrasound, right middle lobe bronchoalveolar lavage, and a biopsy with cultures. The patient had improved clinically on hospital day 6 and was discharged with pulmonology follow-up.One week later, histology revealed lymphocytosis, multiple lipid-laden macrophages, and proliferative fibrosis suggestive of ELP (Image 2). On follow-up phone call, the patient reported complete symptom resolution 2 months after initial presentation. Repeat CT chest showed a decrease in pulmonary nodule size and number. The patient opted to forego biopsy and PET in favor of serial imaging surveillance, with follow up CT scan now planned for December.
Conclusions: ELP should be considered when patients present with an insidious-onset of fevers, dyspnea and a productive cough. Due to its non-specific clinical presentation and radiological features that can mimic other lung diseases, including carcinoma, the diagnosis is often delayed or missed entirely. 30% of patients present with a fever, and nearly 80% have gastrointestinal symptoms such as diarrhea, nausea, and vomiting that can confound diagnosis [1]. Typically, disease progression is halted when exposure to the offending substance is stopped. As in this case, broad spectrum antibiotics are largely ineffective. This patient’s only known exposure to chemicals was an herbicide he used routinely in his work as a landscaper. Our patient denied the use of battery-powered vaporizers, but it is possible that he unknowingly inhaled or aspirated a fatty substance while on vacation, causing this inflammatory reaction. ELP has also been associated with exposure to mineral oil and liquid paraffin, which is used as a laxative, and has traditionally been the most common cause, accounting for ~75% of cases [2].