Background: Point-of-care ultrasound (POCUS) has become increasingly popular in medicine due to its ease of access, reduction in need for consultative ultrasonography, and usefulness in diagnosing common conditions [3,4,5]. The use of POCUS in the inpatient settings of emergency rooms, ICU, Surgical and Medical Wards has been established [3,4,5] The availability of ultrasound machines and handheld devices allows for quick assessment during code blues, rapid responses, and for evaluating patients with hemodynamic instability [5,8]. Utilizing POCUS has been found to lower complications, improve outcomes, and increase patient safety in procedures such as thoracentesis and central venous catheter placement [8]. The application of POCUS in the outpatient setting has also led to reduced times to diagnosis and changes in management [7]. Emergency medicine residents have integrated POCUS training as a requirement [1,2]. However, barriers to establishing a POCUS curriculum for internal medicine residents include limited equipment, number of trained faculty, and time constraints related to patient care [3,5,6]. The goal of this study was to develop a pilot program to assess POCUS knowledge and proficiency via a bootcamp-style education with a focus on 3 common outpatient complaints: leg swelling, shortness of breath, and abdominal pain. The primary endpoint was to objectively identify interest in using POCUS during inpatient and outpatient months throughout residency.
Methods: A POCUS bootcamp was designed for internal medicine post-graduate year 1 (PGY1) trainees’ orientation. 41 PGY1s were provided short lectures on POCUS related to lower extremity venous anatomy and deep venous thrombosis, as well as common respiratory and abdominal pathologies before going to stations. Each ultrasound station consisted of a voluntary human model recruited from the community, a conventional ultrasound machine, and a handheld ultrasound device for each small group of trainees. The objective was to practice using ultrasound to identify vessels, lungs, and anatomy related to the focused assessment with sonography in trauma (FAST) exam. An anonymous test consisting of 13 questions was completed by each resident before and after the intervention. Pretest and posttest results were compared using a paired t-test (statistically significant was a p-value <.05).
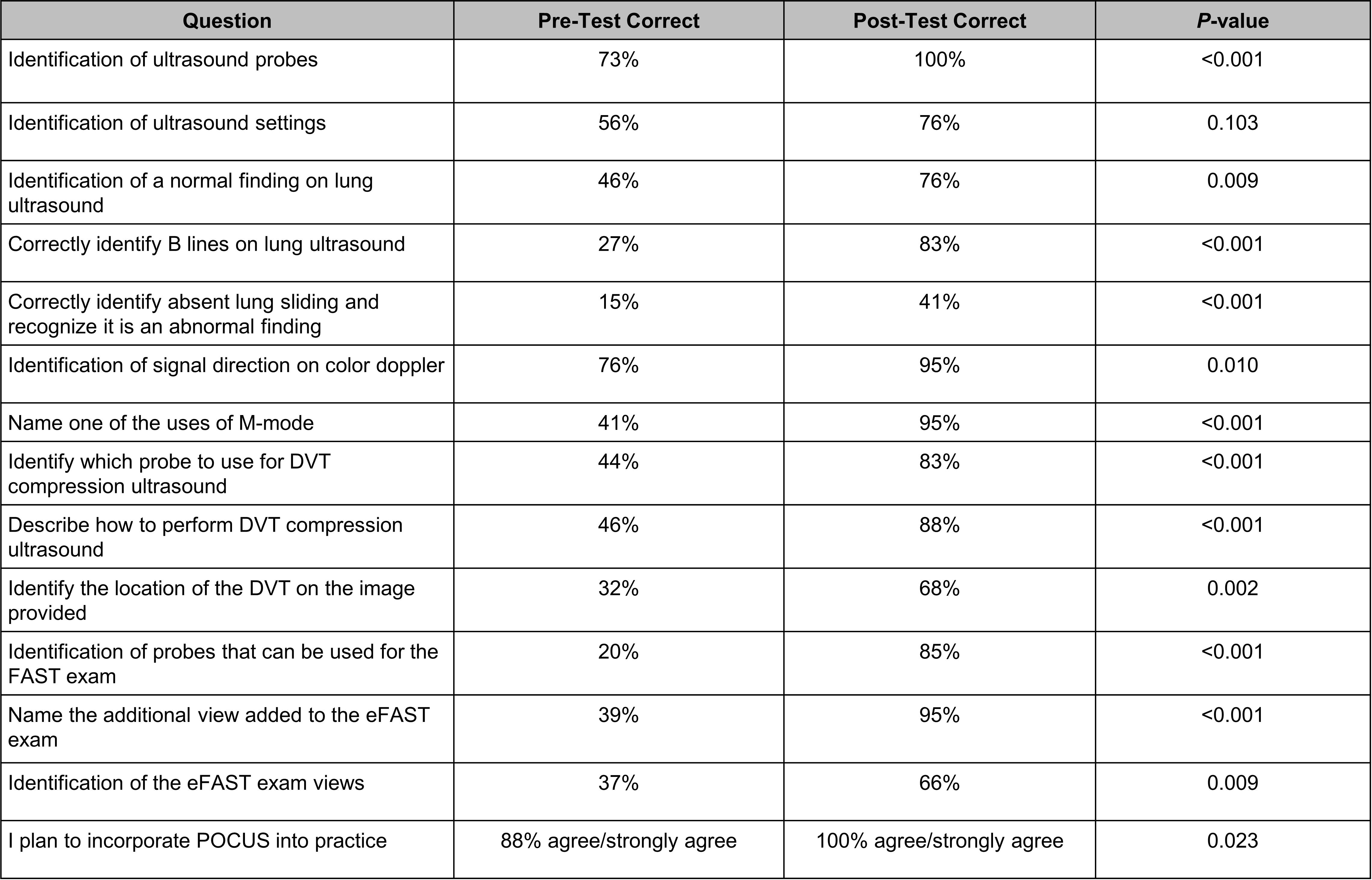
Results: The pretest and posttest correct results were significant in 13 of the 14 questions given, while the question addressing ultrasound settings was not. There was also a significantly higher interest in using POCUS in clinical practice after the bootcamp. Based on feedback, residents overall felt that the bootcamp was helpful when utilizing videos, case examples, and small groups. Areas of improvement included residents needing more practice time and wanting a cardiac ultrasound session.
Conclusions: Internal medicine residents were able to effectively learn the basics of POCUS after brief lectures and practice sessions as evidenced by improvement in a post-didactic assessment. Participants were also more likely to utilize POCUS in their practice after the sessions. Limitations of the study were the small sample size, focus on PGY1 trainees, and inability to assess skills long-term. Future considerations would include another assessment for the same participants at the end of the academic year, teaching cardiac ultrasound and evaluating competency, as well as providing opportunities to obtain formal POCUS certification.