Background: Centers for Medicare & Medicaid Services (CMS) reimbursement increasingly depends on patient satisfaction scores and readmission rates to incentivize high-quality inpatient hospital care. Providers are continuously implementing complementary interventions to improve patient satisfaction and reduce hospital readmissions. Post-discharge phone calls are a relatively simple intervention to implement that can potentially improve continuity of care and reduce readmission risk as patients transition from an inpatient setting to home with home care. Previous research shows a mixed effect of phone call programs amongst physicians, nurses, and pharmacists with multiple explanations as to how this intervention influences patient satisfaction and hospital readmission. Hospitalists at our institution initiated a post-discharge phone call program to evaluate the quality of transitional care through Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores and 30-day readmission rate.
Purpose: To assess the impact of postdischarge phone call from discharging hospitalist on patient satisfaction score with overall hospital care, doctor communication, readmission amelioration, and adherence to follow-up rate.
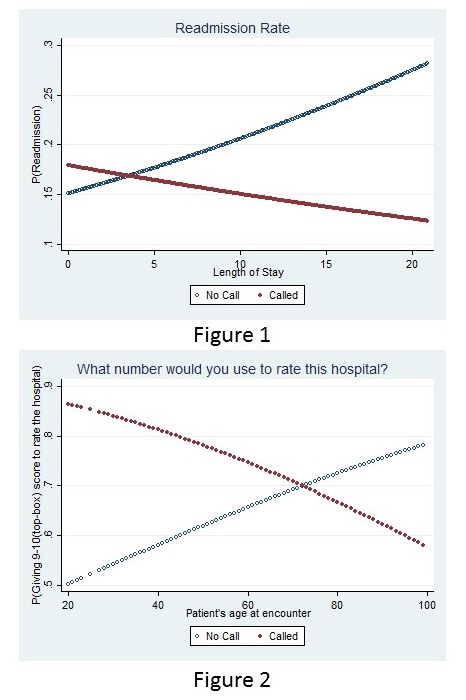
Description: Hospitalists were instructed to call any patient discharged from their service within 7 days of the discharge date. The call was only considered a completed call (and included in study) if the physician spoke to the patient or the patient’s care giver if the patient was felt to have an issues with short term memory. These discharges were to home with self care or home with home care services. Patients discharged to skilled nursing facilities were exclude. Hospitalists were instructed to ask if the patient (or care giver) how patient was doing after recent discharge, had questions about their hospital stay and if they had a follow appointment arranged. Of 4,490 patients included in this study, 1,067 (23.76%) received post-discharge phone calls from a hospitalist. Older patients with severe disease were more likely to receive a phone call. The post-discharge phone call intervention was statistically associated with improvement in the HCAHPS responses for global hospital rating (AOR: 1.52, P = 0.04) and physician communication (AOR: 1.56, P = 0.021) and improvement varied by patient age at first admission (P = 0.001 and P = 0.101, respectively). Patients who received calls were less likely to be readmitted when compared to those with the same inpatient length of stay (Figure 1). Calls for younger age groups had a higher odds ratio of giving top box HCAHPS score than older age groups (Figure 2).
Conclusions: The post-hospital phone call program was significantly associated with a 15% increase in odds of receiving top box HCAHPS scores, which was age-related. Even though the readmission rate was not significantly improved by the phone call intervention, the phone call changed the direction of the association between length of stay and readmission. The underlying reasons for this change should be addressed in further studies.