Background: Medicare Advantage (MA) plans have strong incentives to reduce potentially wasteful healthcare, including costly acute care visits for ambulatory care-sensitive conditions (ACSC) [1-4]. It is unknown, however, whether MA plans lower acute care use relative to Traditional Medicare (TM) or instead shift patients from hospitalizations towards observation stays and emergency department (ED) direct discharges. To the extent that site shifting is occurring, some instances may be appropriate while others may be inappropriate, with unclear effects on care quality. Given MA covers 42% of the Medicare population as of 2021 and enrollment is expected to continue growing [5], it is critical to understand such differences.
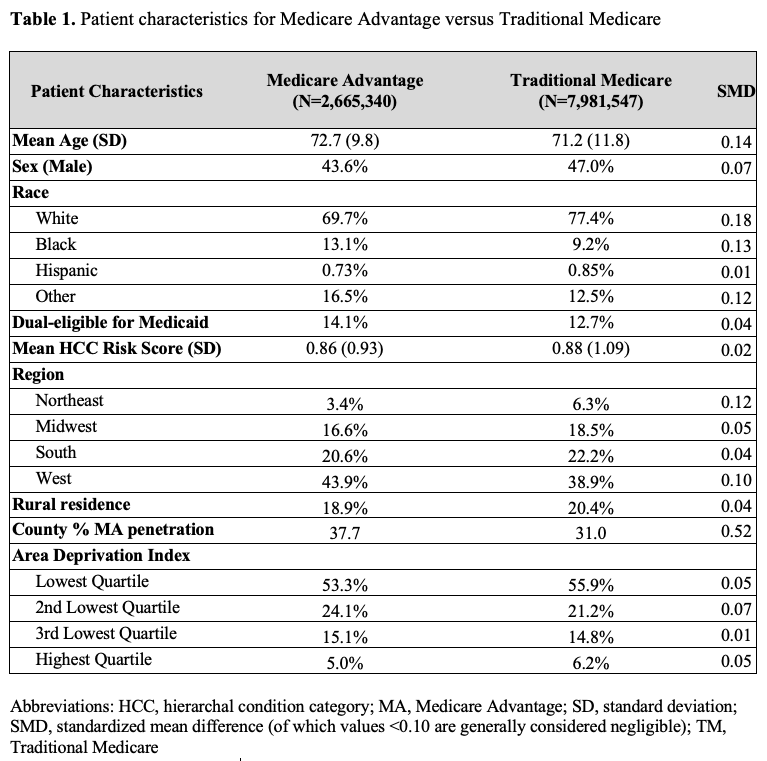
Methods: Objective: To determine whether MA is associated with differential utilization of hospitalizations, observations, and ED direct discharges for ACSCs compared to TMDesign: Cross-sectional study from January 1 to December 31, 2018 using Poisson regression models to compare risk-adjusted rates in MA vs. TM, controlling for patient demographics, clinical risk, and including county-fixed effects.Setting: U.S. Participants: MA vs. TM beneficiaries Main Outcome Measures: Hospitalizations, observation stays, and ED direct discharges for ACSCs
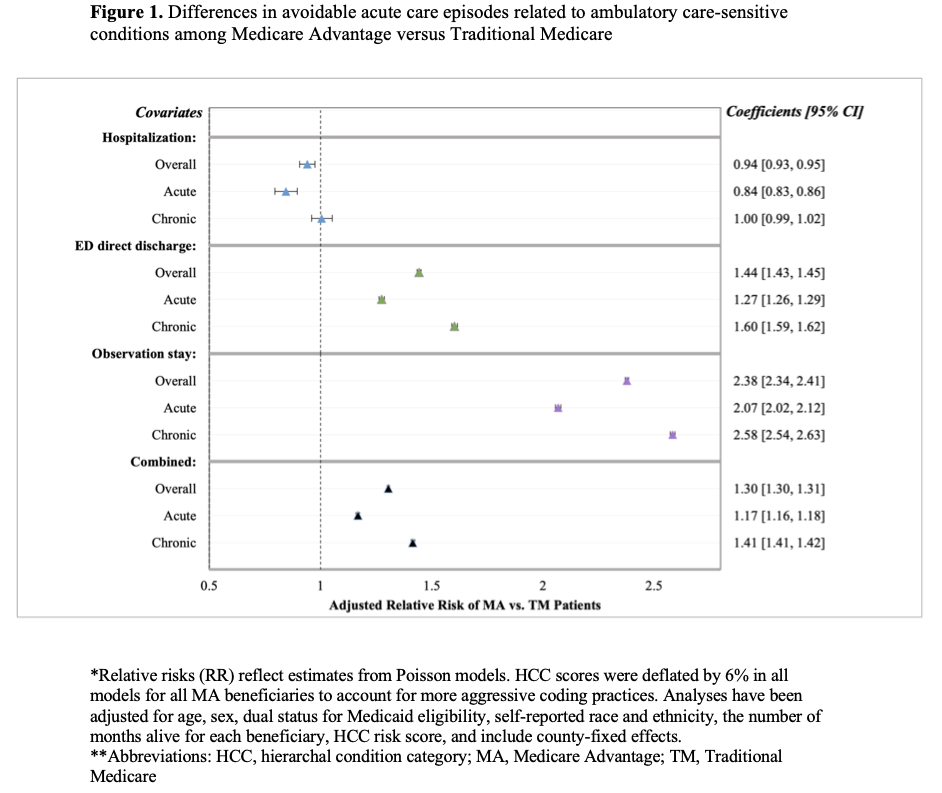
Results: Results: Among 2,665,340 MA patients and 7,981,547 TM patients, MA patients had lower risk of hospitalization for ACSCs than TM patients (relative risk [RR] of 0.94; 95% CI, 0.93 to 0.95), primarily driven by fewer hospitalizations for acute conditions (e.g. pneumonia). Patients in MA had higher risk of ED direct discharges (RR 1.44; 95% CI 1.43 to 1.45) and observation stays (RR 2.38; 95% CI 2.34 to 2.41) related to ACSCs vs. TM. Overall, patients in MA were at higher risk of needing care for an ACSC–including hospitalization, ED direct discharge, or observation stay–than patients in TM (RR 1.30, 95% CI 1.30 to 1.31). Within the MA population, patients in MA HMOs were at lower risk of ACSC hospitalization compared to patients in MA PPOs (RR 0.96; 95% CI 0.95 to 0.98;), but MA HMOs had a higher risk of ED direct discharge (RR 1.08; 95% CI 1.07 to 1.09) and observation stay (overall RR 1.10; 95% CI 1.02 to 1.12).
Conclusions: In this national study of MA and TM patients, apparent gains in reducing potentially avoidable acute care among MA plans were explained by shifting inpatient care to other settings–such as ED direct discharges and observation stays–rather than delivery of higher-quality outpatient ambulatory care.