Background: Observation status was designed to reduce health care costs for patients in need of short hospital stays. CMS suggests that observation care should typically require less than 24 hours, and only rarely last more than 48 hours. However, studies suggest that length of stay for observation patients is often longer than CMS guidance.[1,2] An observation unit filled with patients who are long stay (>24hours) are mismatched for the competency of a high turnover observation unit. Correctly identifying short-stay observation status patients at the time of emergency department (ED) disposition decision should reduce hospital denials and improve operations by reducing internal transfers, avoidable handoffs (physician/nursing), ED boarding time and inappropriate utilization of environmental services.
Methods: Our ED is currently using a machine-learning-based clinical decision support (CDS) tool for triage. The tool predicts patient’s risk of critical care, emergency procedure, and hospitalization using routinely available ER triage data: complaints, vital signs, demographics, and past medical history.[4, 5] Risk is translated to triage level recommendations that may be accepted or overridden by the triage nurse. We aim to use this same tool with collaboration of our physicians to predict the likelihood of hospitalization less than 24 hours. We performed a retrospective observational study and applied this CDS tool to a cohort of adult ED patients triaged at a community-based hospital between January 1, 2018 and September 1, 2019. Those hospitalized were eligible to receive the decision support. The major outcome was predicting the likelihood of a patient being in the hospital < 30 hours from arrival (6 hours ED LOS + 24-hour hospitalization). Performance measures, AUC, sensitivity, specificity all evaluate out-of-sample using 5-fold cross-validation.In this new workflow, upon decision to hospitalize, our hospitalist would still have the ability to change the patient status from ER to Observation or Inpatient. If meeting short-stay criteria, a CDS message would be displayed in the Electronic Health Record to place the patient in both observation status and in our observation unit. Our provider has final discretion on this decision.
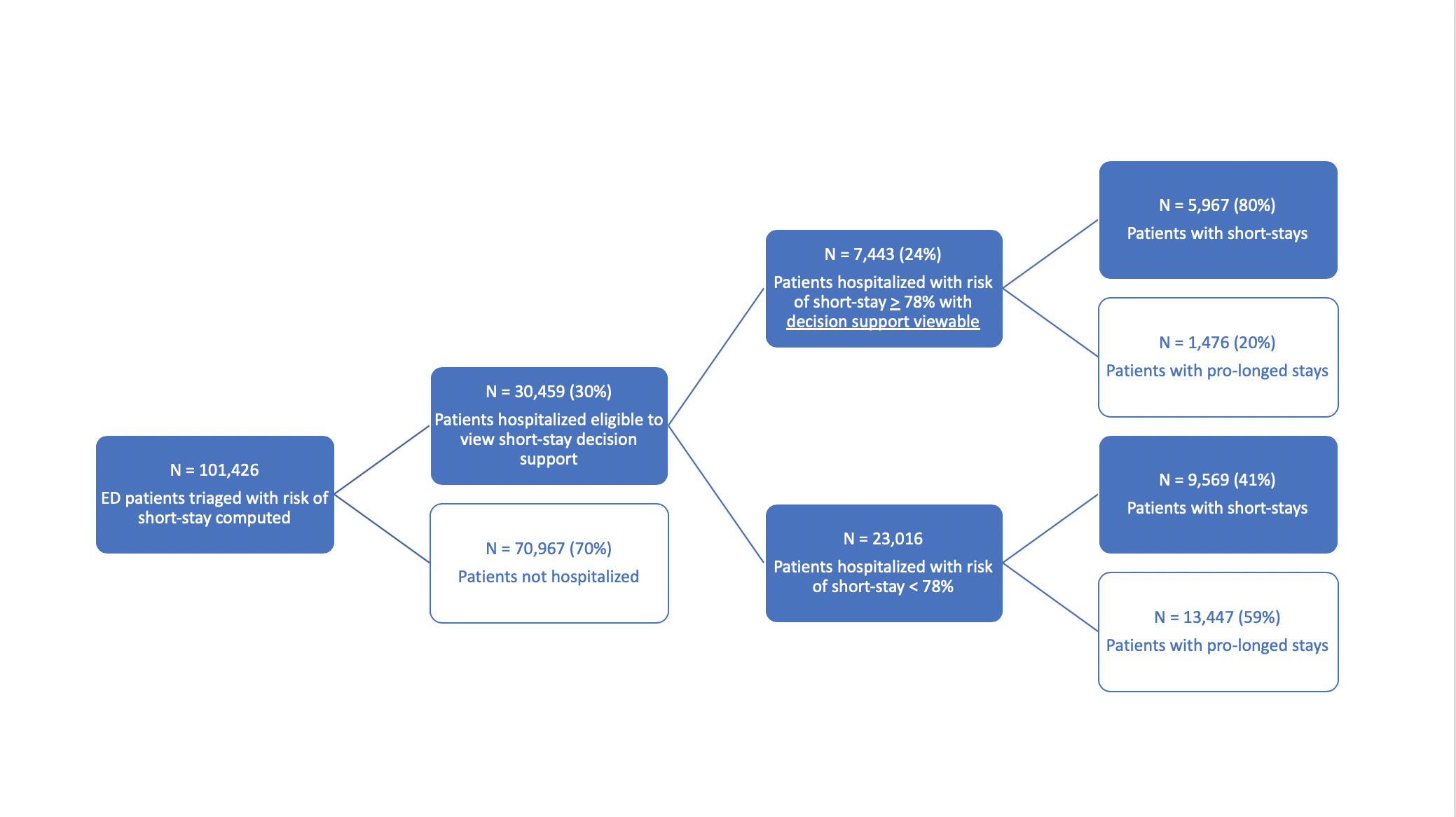
Results: Applying our model to a cohort of 101,426 adult ED patients triaged at Howard County General Hospital, ultimately 30,459 (30%) were hospitalized and eligible to receive the decision support as seen in Figure 1. Of those hospitalized, 15,536 (51%) were short-stays. The AUC for predicting short stay patients at ED triage was 0.82. Selecting a 78% risk of short-stay threshold, an estimated 7,443 (24%) of hospitalized patients would receive a viewable warning that the patient is likely short-stay. This would represent and estimated 38% sensitivity and 80% specificity in accurately identifying short-stay patients.
Conclusions: By utilizing a clinical decision tool that identifies patients who will stay in the hospital less than 24 hours, we are able to correctly identify short stay observation patients as well as preferentially place these patients in an observation unit designed for high turnover. More than 40% of all nurse case manager job postings are now for status determination work, shifting duties from patient care and quality improvement.[3] This tool shows potential for improved predictive performance over the resource intensive use involved to make this decision more accurate and cost effective.