Background: Bed-rest is considered essential to recovery. Functional decline in older patients is an often-overlooked riskfactor during hospitalizations. Older patients have higher 30-day readmission rates, more complications,and longer lengths of stay. Increasing the amount of walking in the hospital has been identified as a potentialsolution, with 900 steps per day identified as a target to prevent hospital-associated functional decline (HAFD)(Agmon 2017). Our objective was to incorporate wearable activity trackers to discover the amount of activity patients aregetting in the hospital during their inpatient stay and to understand if promoting in-hospital mobility is relatedto their length of stay and discharge disposition.
Methods: The randomized control trial was conducted in acute medicine inpatient units in two New York University Langone Health hospitals in Manhattan and Brooklyn.The study ethical review process through the institutional review board was 2 months, and patients were recruited over 8 months. Designated research team members conducted chart reviews for potential patients through the electronic health records, approached and completed an informed consent with patients who were interested to participate in the study. All participants enrolled in the study wear required to wear activity trackers to track daily steps. The intervention arm was reminded to walk twice daily with either text messages or silent vibrations through the tracker, and the control arm did not receive any reminders. We assessed the differences in means using the Mann-Whitney test to determine associations between daily steps and LOS, discharge disposition and intervention.
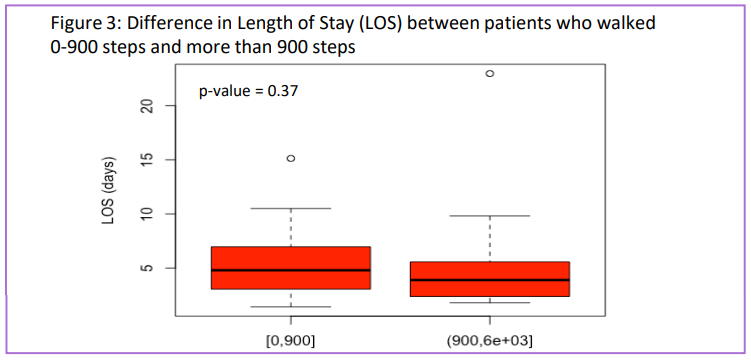
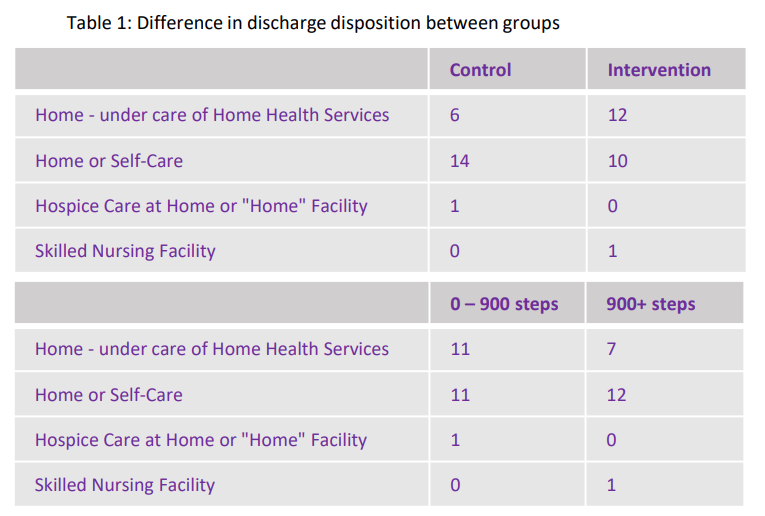
Results: Fifty one participants were recruited for the study and 44 were assessed. In total, the average number of steps was 973.67, with a median of 581.1 steps. The average number of steps per day for the control group was 573.58 (SD 820.15). The average number of steps per day for the intervention group was 934.95 (SD 1506.38). There were no statistically significant differences in daily steps between the control and intervention groups, length of stay, or discharge disposition.
Conclusions: While there were no statistically significant differences in daily steps between the study arms, LOS, or dischargedisposition, the lessons learned in this pilot study can be extrapolated to a grander stage leading to betterrecruitment and evaluation of hospital mobility, as it is already known that maintaining mobility into advancedage improves function. This study increases awareness in the patient population to ambulate as much as possible during their hospital stay and fostered conversations in hospital staff and leadership members to increase in-patient mobility across the hospital.