Background: Diagnostic errors (DEs) represent ongoing threats to patient safety in the hospital. Little is known about the factors present on admission that can predict DE during the hospital encounter. Such knowledge is essential for prospective identification of hospitalized patients at risk for DE who can be targeted for early intervention. The purpose of this study was to conduct a secondary analysis of a stratified sample of cases from three high-risk cohorts to identify potential predictors (Table 1) of DE during the hospital encounter.
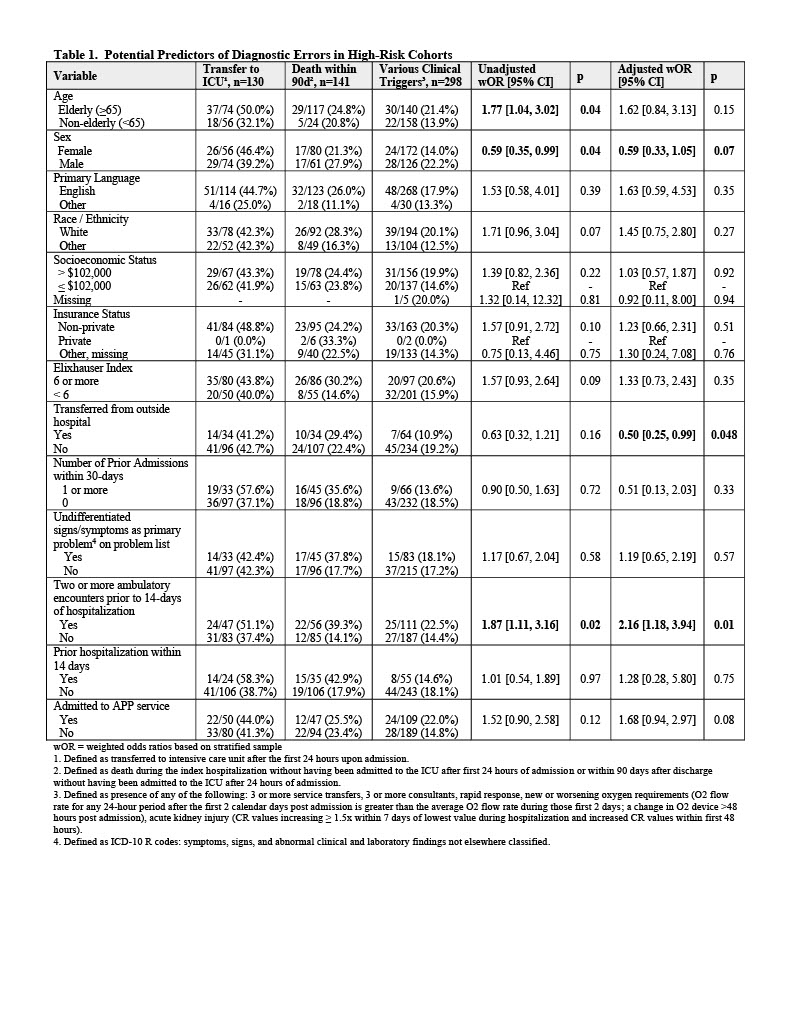
Methods: Our sample cohort included patients hospitalized on the general medicine service at a tertiary academic medical center in Boston, MA. We previously used a structured chart review process utilizing the SAFER Dx instrument and 2-clinician adjudication to determine the likelihood DE in each case.1 A total of 569 cases with adjudicated outcomes (141 DE positive, 428 DE negative) were sampled from 4750 available cases across three high risk cohorts (number, % of available cases sampled): transfer to the intensive care unit (ICU) after 24 hours (n=130, 100%); death during hospitalization and within 90-days of discharge (n=141, 38.5%); and various clinical triggers (n=298, 6.8%) which included multiple transfers, multiple consultants, new or worsening oxygen requirement, rapid response, and acute kidney injury (see Table 1, footnote 3). Multivariable logistic regression, adjusting for all covariates, was used to model the outcome (DE in the primary or secondary diagnosis) and calculate the c-statistic. Weighted odds ratio (wOR) and 95% CI were calculated for the cohort in both unadjusted (bivariable) and adjusted (multivariable) analyses.
Results: In multivariable analyses, two or more ambulatory encounters within 14-days prior to hospitalization (adjusted OR [95% CI] 2.16 [1.18, 3.94], p = 0.01) was significantly associated with DE. Transfer from an outside hospital was significantly inversely associated with DE (adjusted OR [95% CI] 0.50 [0.25, 0.99], p = 0.048). Sex and admission to the advanced practice provider (APP) service trended towards significant association. The multivariable model yielded a c-statistic of 0.66.
Conclusions: Potential predictors of DE in hospitalized patients in this high-risk cohort included multiple ambulatory encounters prior to hospitalization (indicative of diagnostic uncertainty), and possibly sex and admission to the APP service. Interestingly, interhospital transfer, often implicated in safety events, was a protective factor, suggesting transfer into our hospital was for advanced therapeutic interventions (when the diagnosis is known) or heighted awareness of uncertainty prompted a more thorough diagnostic process. The discriminative ability of our prediction model was suboptimal; additional variables and analyses on larger cohorts are required. Once more thoroughly validated, such prediction models may be useful for prospectively identifying patients at risk for DE during hospitalization.