Background:
Catheter occlusion is often encountered when using peripherally inserted central catheters (PICCs). Patients who experience catheter occlusion are at risk of interruption of therapy, thrombolytic instillment, and complications such as VTE. Whether rates of PICC occlusion vary by flushing protocols, device type, or duration is not known.
Methods:
Using data from the Michigan Hospital Medicine Safety Consortium (a multi-hospital quality improvement initiative dedicated to preventing adverse events in hospitalized medical patients), we examined prevalence and variation of PICC occlusion in hospitalized medical patients in 47 hospitals. Descriptive statistics were used to tabulate rates of occlusion across participating sites. Chi-square tests were used to test for differences in unadjusted rates. Mixed-effects logistic regression was then used to adjust for duration of use (days), device characteristics (lumens and gauge), and hospital protocols for flush type (normal saline, heparin, or both) and flush frequency (daily, BID or TID). Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) were generated.
Results:
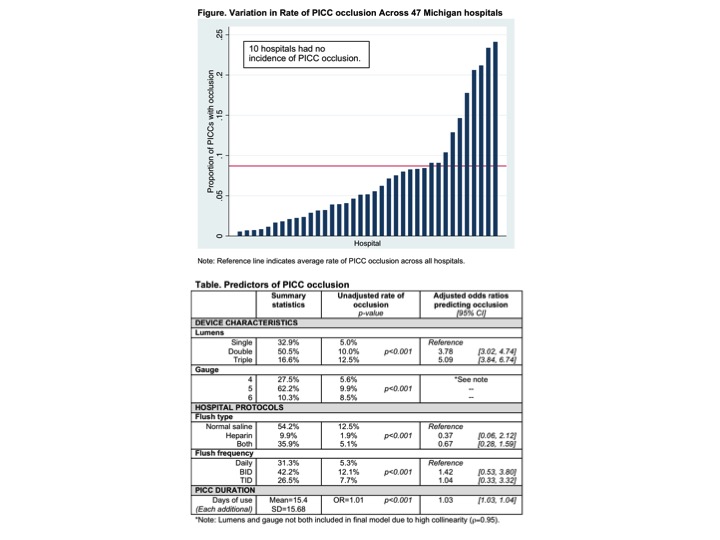
Of 10,168 PICCs available for analysis, 885 (8.7%) developed occlusion. Most devices (68.2%) were placed by vascular access nurses, but cared for by bedside nurses following insertion. tPA was often used to treat occlusion (N=748; 84.5%) but 81 devices (9.1%) required removal. Rates of PICC occlusion varied substantially across hospitals, from 0% to 24.1%, was noted across hospitals (Figure).
Unadjusted rates found PICC occlusion occurred more frequently with double and triple lumen catheters; when devices were flushed with only saline compared to heparin or both; and when devices were flushed BID, compared to daily or TID. In multivariable analyses, double and triple lumen devices were associated with increased odds of occlusion (OR=3.78 [CI=3.02, 4.74] and 5.09 [CI: 3.84, 6.74] respectively) compared to single lumen devices. Each additional catheter day also increased the odds of occlusion (OR=1.03 [CI=1.03, 1.04]). Differences in flush type and frequency were not significant. (Table).
Conclusions:
PICC occlusion is common and is associated with device characteristics and duration of use. To better understand nursing practices to prevent occlusion, qualitative and quantitative approaches appear necessary.