Background: Medicine procedure services (MPS) increasingly perform bedside procedures such as lumbar puncture (LP). While rates of major complications are low, success rates in the literature are widely variable and dependent on patient body habitus, patient positioning, operator experience, and use of ultrasound guidance.1 Many trainees report discomfort with their skill in performing and supervising bedside procedures, in particular lumbar punctures. Overall success rates and factors associated with LP success performed by MPS have not been well described. Our aims included: 1) description of overall success and outcomes of LPs performed by a MPS with and without ultrasound and 2) identification of factors associated with successful or traumatic LPs.
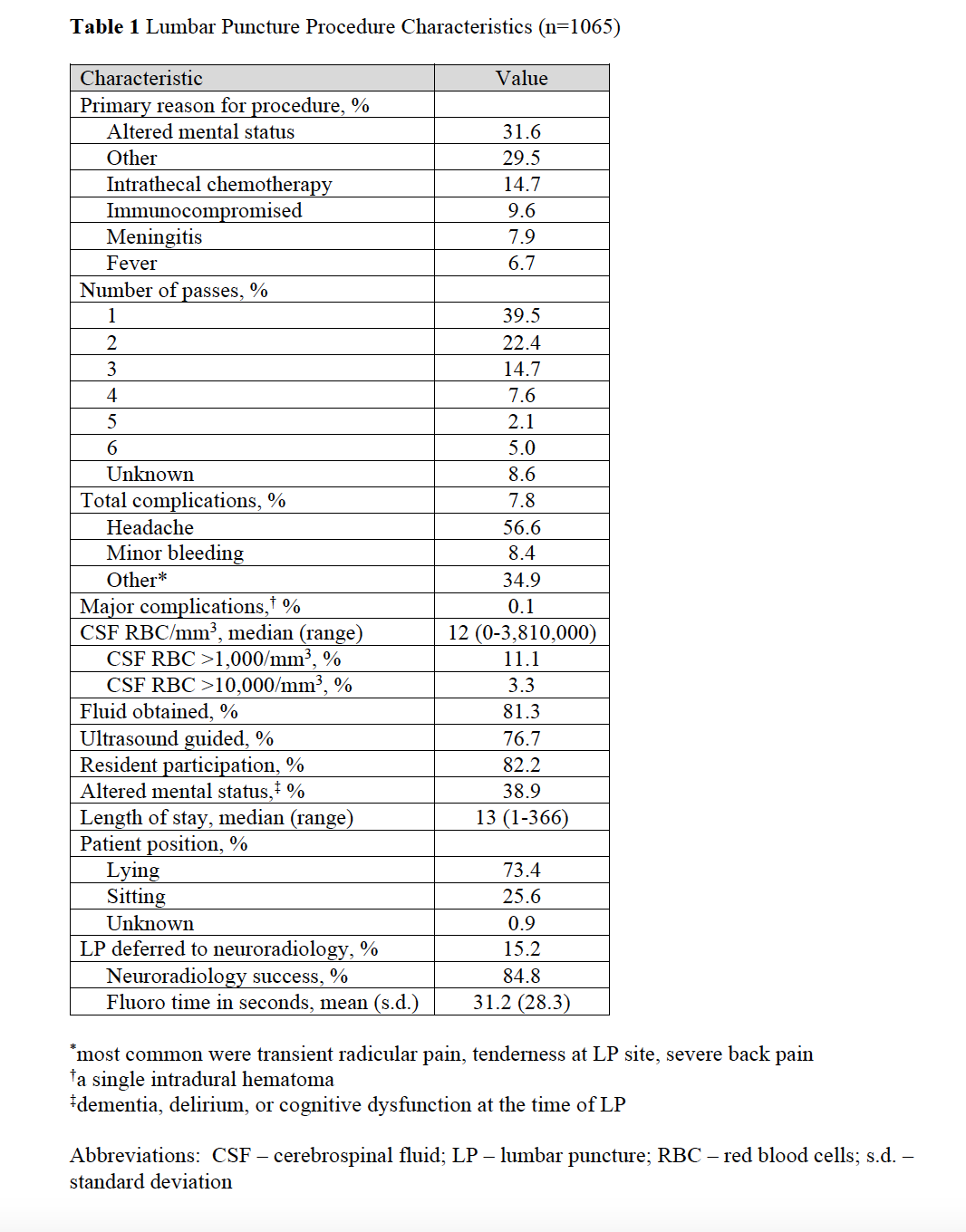
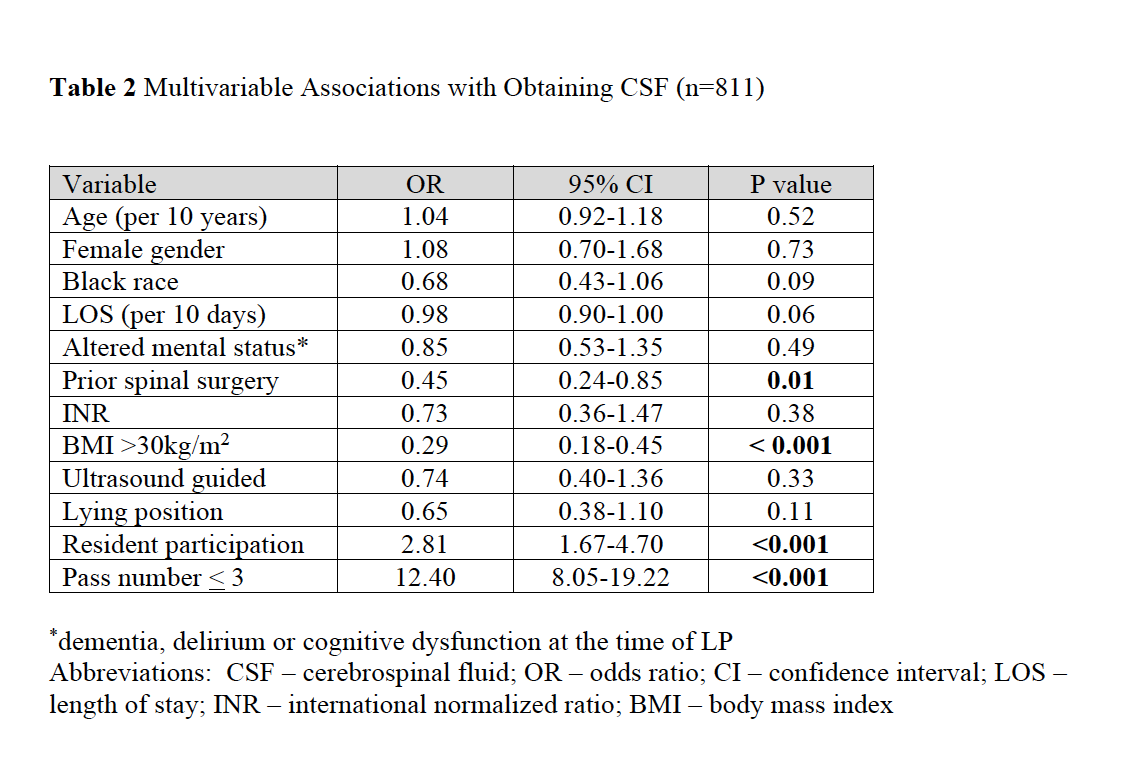
Methods: We performed a longitudinal study of patients undergoing LP by a MPS September 2015 to December 2020. We identified demographic and clinical factors, including age, gender, race, body mass index (BMI), presence of altered mental status, history of spinal surgery, use of ultrasound, referral to neuroradiology and trainee participation. Demographic data were imported directly from the electronic medical record and clinical variables were obtained via a standardized chart review. Outcome measures included proportion of successful LPs, defined as obtaining any amount of CSF, the proportion of LPs that were traumatic, defined as CSF red blood cell (RBC) count greater than 1,000/mm3 and any procedural complications. Among unsuccessful LPs, we measured the number of referrals to neuroradiology. We also performed multivariate analysis to identify factors associated with LP success and traumatic LP. Only encounters with complete data for all variables were included in the multivariate analysis.
Results: We identified 1,065 LPs among 844 patients. Trainees participated in 82.2% and ultrasound was used in 76.7% of LPs. Overall success rate was 81.3% with 7.8% having minor and 0.1% major complications. A minority of procedures were referred to neuroradiology (15.2%) or were traumatic (14.4%). Of the cases referred, subsequent success rate was 84.8%. There were 811 patients with complete data for multivariable analysis. In that analysis, BMI >30 kg/m2 (OR 0.29, 95%CI 0.18-0.45) and prior spinal surgery (OR 0.45, 95%CI 0.24-0.85) were associated with decreased odds of successful LP; trainee participation (OR 2.81, 95%CI 1.67-4.70) and < 3 needle passes (OR 12.4, 95%CI 8.05-19.22) were associated with increased odds of success. Ultrasound guidance (OR 0.48, 95%CI 0.31-0.76) and < 3 needle passes (OR 0.50, 95%CI 0.32 – 0.77) were associated with lower odds of traumatic LP.
Conclusions: In a large cohort of patients undergoing LP by a MPS, many patients had a successful bedside procedure with a low complication rate. A minority of lumbar punctures were referred to radiology. With coaching from experienced proceduralists, trainee participation was associated with increased odds of success, while obesity and prior spinal surgery were associated with decreased odds. Ultrasound guidance was associated with lower odds of traumatic LP. Our data may help guide institutions in determining best structures for performing, referring, and teaching LP procedure skills. Individual practitioners may also use this data for pre-procedural planning and patient counseling regarding procedural risks, benefits, and likelihood of success.