Background: Overuse of daily labs (DL), especially CBC and BMPs in hospitalized patients leads to increased costs and utilization of resources, iatrogenic anemia, and patient discomfort. Prior quality improvement (QI) efforts in hospital medicine have worked to reduce excessive lab utilization, but few have focused on labs ordered on the day of discharge (LOD) . LOD in medically stable patients are often unnecessary and may prolong length of stay (LOS) . Furthermore, those awaiting discharge to post-acute care such as skilled nursing facilities (SNFs) may represent an important group of patients at risk of receiving unnecessary DL and LOD due to frequent non-medical delays in discharge. This study aimed to assess the prevalence of DL and LOD for patients discharged to SNFs. We also examined associations of DL and LOD with provider and hospitalization characteristics.
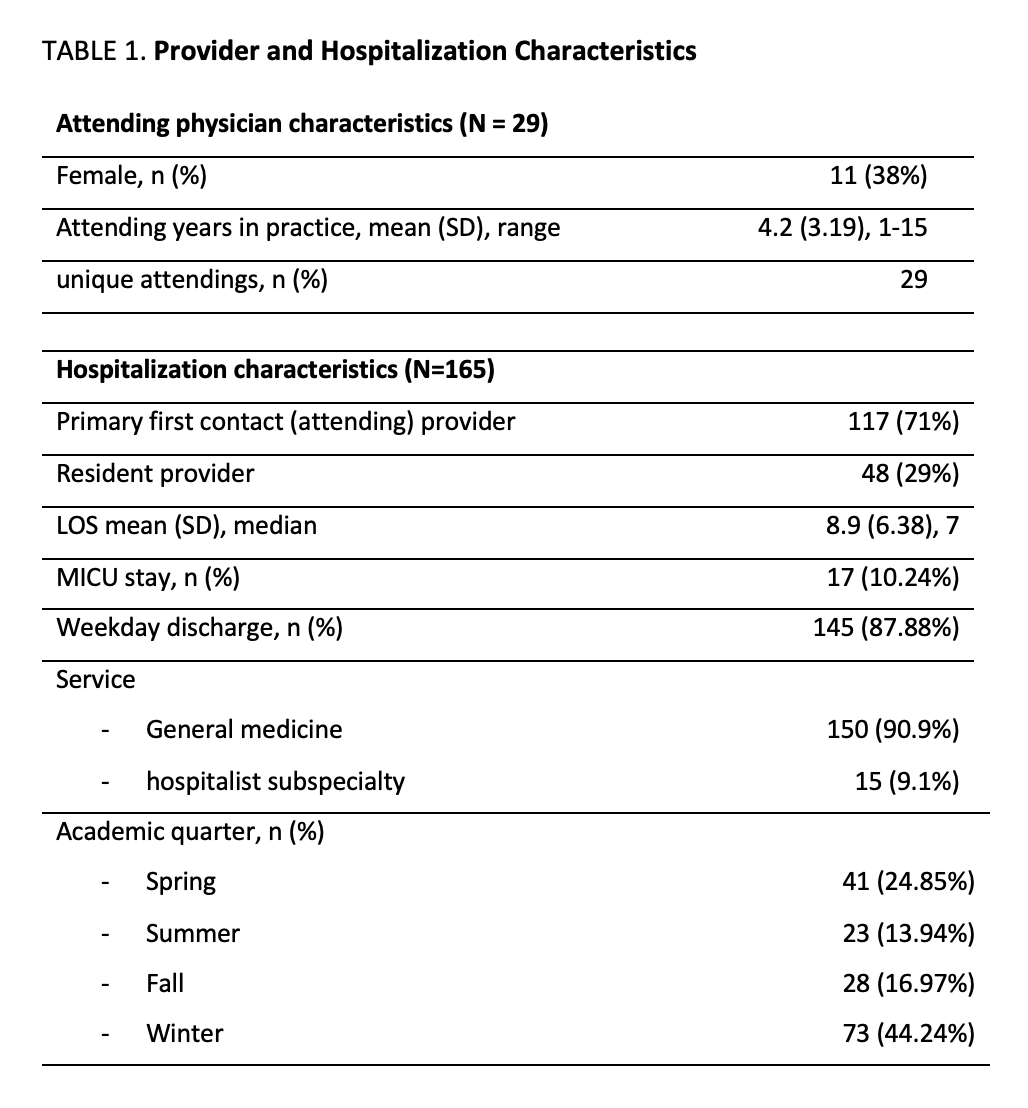
Methods: This study was a retrospective analysis of patients on 2 University of Chicago, a 600-bed urban, academic, tertiary referral center, direct-care services staffed by an attending hospitalist and internal medicine third-year resident (PGY3). Each provider is primary physician for 7 patients; the attending hospitalist supervises the care of all 14 patients. DL and LOD ordering data were extracted for all patients discharged from these services to SNFs from 1/1/2021-12/31/2021. Our primary outcome was prevalence of DL and LOD, defined as BMP and/or CBC present every day of hospitalization including discharge. We performed bivariate and stepwise multivariate logistic regression to determine if DL and LOD ordering practices varied between provider characteristics (i.e., attending vs resident providers, hospitalist gender, years of hospitalist experience); or hospitalization characteristics (i.e., weekday vs weekend discharge, patient specialty type, academic quarter, patient LOS, and presence or absence of ICU stay during hospitalization).
Results: 165 encounters met inclusion criteria. 91% (150/165) of patients had DL and 73% (121/165) had LOD. 71% (117/165) had attendings as the primary provider and 29% (48/165) had residents. In bivariate analysis, there were no significant differences in LOD by provider characteristics. However, among patients with ICU stay, 94% (n=16) had LOD compared to those without ICU stay (71%, n=105, chi2=4.19, p = 0.041). Likewise, patients on subspecialty services had proportionally more LOD (100%, n=15) than general medicine patients (70%, n=106, chi2=6.0, p = 0.014). In stepwise regression, no one factor was statistically significant, although patients with ICU stay had about seven times higher odds of having LOD (OR=6.98, 95% CI[0.84-57.8, p=0.07).
Conclusions: For patients discharged to SNF, use of LOD and DL was high. There was an association between higher acuity measures (such as subspecialty patients and ICU stay) and increased prevalence of LOD and DL, although this effect was not seen in multivariate regression. Given these findings, variability in lab ordering may be explained by unmeasurable factors not specific to patient- or provider-related characteristics. Next steps will include sampling a larger subset of patients and determining whether LOD were appropriate to guide stepwise QI implementation of interventions to reduce over-utilization of LOD in patients awaiting SNF. Our findings suggest efforts should be broad-based, targeting all ordering providers and patients.