Background: Accountable Care Units (ACUs) with Structured Interdisciplinary Bedside Rounds (SIBR® rounds) have shown significant improvements in throughput, clinical outcomes, and satisfaction. Yet, prior studies have noted difficulties achieving such improvements or sustaining them. Interdisciplinary rounds are a predominantly physician-led teamwork process with efficacy vulnerable to inconsistent physician leadership and engagement. Our hospital had previously implemented ACUs and SIBR, with variable physician and nurse performance and engagement barriers to sustained improvements. SIBR degraded over time, exacerbated by the COVID-19 pandemic. In 2022 we began to relaunch our ACUs with SIBR rounds to align unit outcomes with organizational goals: improved length of stay (LOS), discharge coordination, and patient experience. With this relaunch, we sought to optimize process fidelity and outcomes by (1) measuring performance variation and (2) coaching outlier physicians.
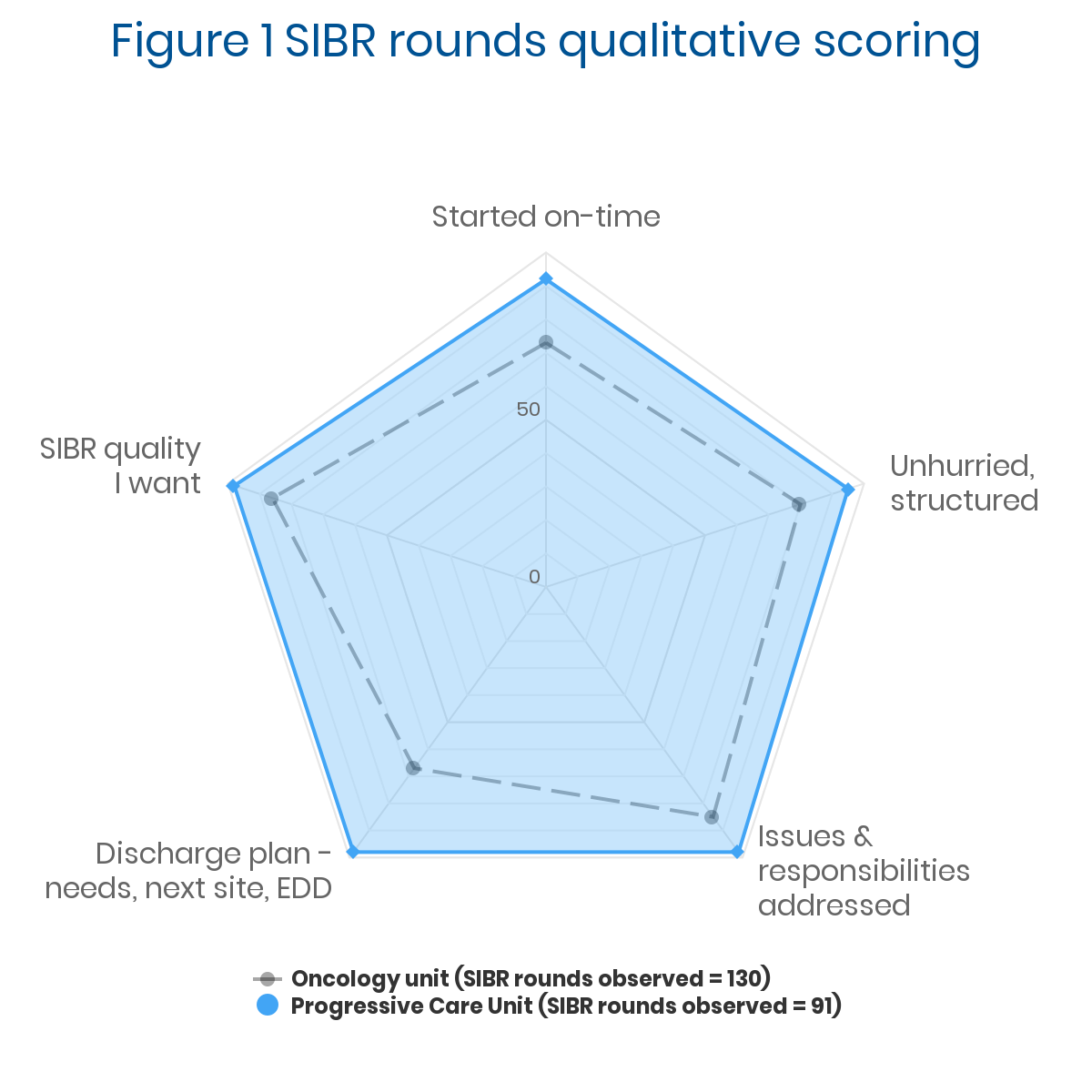
Methods: We relaunched SIBR on a 17-bed oncology unit and 15-bed Progressive Care Unit (PCU). Project leadership, training, and tools were provided by external experts. We used a novel strategy to measure, report, and act on daily performance data: 1. Measure: The charge nurse managing the round (a) tracked quantitative activity and (b) rated team performance against five criteria. 2. Report: A unit clerk digitized the data, feeding automated physician, team, and unit performance reports. 3. Act: Physician and nurse leaders reviewed reports at weekly meetings to identify and address issues.
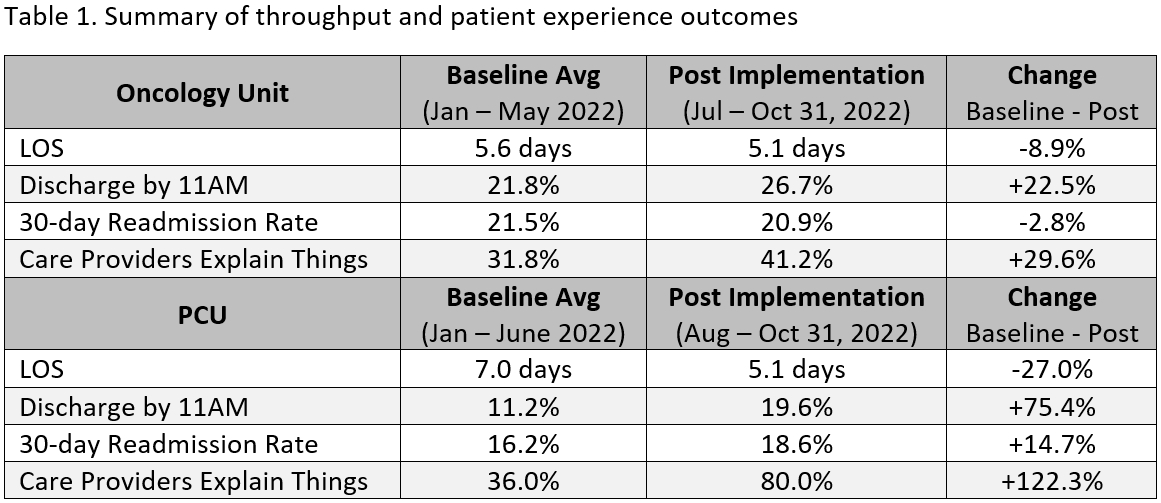
Results: We relaunched SIBR on a 17-bed oncology unit and 15-bed Progressive Care Unit (PCU). Project leadership, training, and tools were provided by external experts. We used a novel strategy to measure, report, and act on daily performance data: 1. Measure: The charge nurse managing the round (a) tracked quantitative activity and (b) rated team performance against five criteria. 2. Report: A unit clerk digitized the data, feeding automated physician, team, and unit performance reports. 3. Act: Physician and nurse leaders reviewed reports at weekly meetings to identify and address issues.
Conclusions: So far, we have seen strong improvements in length of stay, discharge by 11am, and the HCAHPS criterion ‘Care providers explain things,’ consistent with the literature. Process monitoring enabled leaders to rapidly remediate performance variability. We believe this system could be used elsewhere. As we continue relaunch, we will further analyze whether this novel performance monitoring strategy enhances sustainability. If so, it could remove a key barrier to the broader spread of interdisciplinary rounds, significantly benefitting inpatient populations.