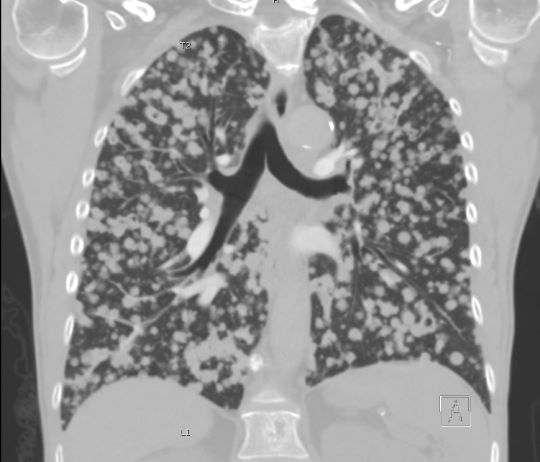
Case Presentation: A 56-year-old smoking female presented to the emergency room with a two-month history of progressive shortness of breath, dry cough, and unintentional weight loss. Her vital signs included a temperature of 36.4°C, heart rate of 116 beats/minute, and a respiratory rate of 24 breaths/minute. Her general appearance was a thin and cachectic woman with a hoarse voice. She did not have cervical or axillary lymphadenopathy or palpable thyroid masses. Her lungs were clear to auscultation bilaterally. Chest x-ray revealed bilateral innumerable nodules that had replaced the normal lung parenchyma. Computed tomography (CT) of the chest showed solid and cavitated nodules of varying sizes with a random distribution and multiple vertebral lesions (Figure 1A). An abdominal CT revealed multiple liver lesions, prominent gonadal veins, and left adrenal thickening. Brain magnetic resonance imaging (MRI) demonstrated a few supratentorial enhancing foci within the left parietal bone. Although suspicion for infection was low, three sputum were obtained for acid-fast bacilli (AFB) and were all negative. We were then consulted on the pulmonary service, a bronchoscopy with transbronchial lung biopsies was performed, and the pathology of these biopsies resulted as thyroid transcription factor-1 positive, cytokeratin 7 positive, cytokeratin 20 negative, homeobox protein CDX-2 negative primary lung adenocarcinoma. Further molecular analysis detected the presence of an epidermal growth factor receptor (EGFR) gain of function deletion at exon 19. She was subsequently discharged home and received one cycle of Carboplatin with Pemetrexed before switching to Osimertinib. Four months later her lung, liver, and brain lesions were significantly improved on imaging and remained stable at her most recent follow-up imaging at seven months (Figure 1B).
Discussion: Lung cancer is the leading cause of cancer-related death in the world in both men and women [1]. The typical radiographic findings of primary lung cancer are a solitary nodule or mass, whereas metastasis to the lung more commonly presents as multiple or bilateral pulmonary nodules [2]. Our patient’s innumerable pulmonary nodules initially appeared more consistent with metastasis to the lung, but pathology confirmed that it was of primary lung origin. Driver mutations such as EGFR mutations have been shown to have a higher association with lung adenocarcinoma presenting with multiple pulmonary nodules when compared to lung adenocarcinoma without driver mutations [3]. This patient’s lifelong smoking history and driver mutation likely interacted in a synergistic manner, increasing her risk for developing primary lung cancer at a relatively young age and in such a diffuse fashion.
Conclusions: We present a rare case of primary lung adenocarcinoma presenting as innumerable pulmonary nodules. This case highlights several important points. First, primary lung cancer can present as multiple pulmonary nodules. Second, smoking and EGFR mutations are significant risk factors for lung cancer and likely contributed to this patient developing such diffuse disease at a relatively young age. Lastly, we highlight the importance of driver mutations in patients with lung cancer, as demonstrated by our patient’s significant improvement of her lung nodules following EGFR targeted therapy.