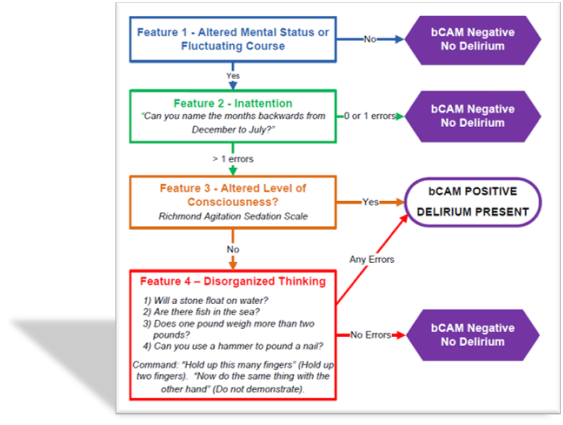
Background: Delirium is an acute state of brain failure marked by sudden onset of confusion, a fluctuating course, inattention, and often an abnormal level of consciousness. Delirium affects about 11-40% of the hospitalized patient population. In hospital delirium has been associated with 10-fold increased risk for death and a 3-to-5 fold increased risk for nosocomial complications, prolonged length of stay, and greater need for nursing home placement after discharge(1). Although delirium is common, studies show that in affected persons, delirium is recognized by only about one-third of physicians and about one-third of nurses. The Brief Confusion Assessment Method (BCAM), developed by Han et al is an adaption of Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) both of which are based on the Confusion Assessment Method (CAM)(2, 3). In contrast to CAM, which takes at least five minutes to be completed, BCAM can be performed in less than one minute. BCAM has previously been validated in ED population, where it showed Sensitivity of 84.0%, with 95.8% Specificity(2, 4). Our study is a validation study comparing BCAM against the gold standard CAM in general medicine inpatient population.
Methods: The study was designed as prospective observational study to validate BCAM against CAM in general medicine inpatient unit. This study was carried out in 50-bed general medicine inpatient unit with high volume geriatric admissions. Inclusion criteria: Patients enrolled were from March 1, 2020 – November 15, 2020. All patients admitted to the inpatient unit 65 years or age or older were assessed with BCAM every shift and with any new change in mental state. Exclusion criteria: Patients were excluded if they were non-English speaking, deaf or blind, comatose, non-verbal or unable to follow simple commands prior to admission as determined by medical record review and discussion with bedside nurse. The BCAM was performed by the bedside registered nurses. All nurses received extensive BCAM evaluation training. Gold standard CAM assessment was performed by internal medicine physicians and or geriatricians within three hours of first BCAM assessment.
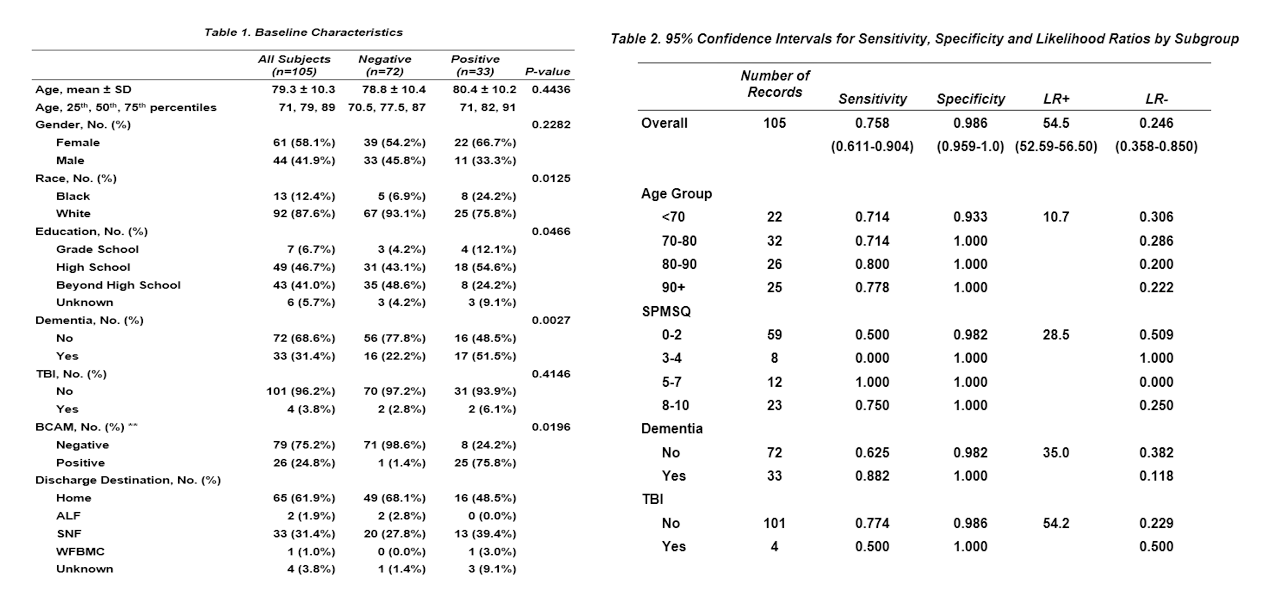
Results: Data analysis was done using SAS 9.4 software. A total of 105 patients were enrolled in the study. Mean age of the patients was 79.3 ± 10.3 years (p=0.4436) with female 58.1% and male 41.9% (p=0.2282). When compared with CAM, delirium was present in 26 (24.8%) of the 105 patients (p=0.0196). The BCAM showed sensitivity of 75.8% (95% CI, 0.611-0.904 ) and specificity of 98.6% (95% CI, 0.959-1.0 ). Positive and Negative likelihood ratio (LR) were 54.5 (95% CI, 52.59-56.50) and 0.246 (95% CI, 0.358-0.850) respectively. Covariate analysis: 33 (31.4%) patients had documented dementia. BCAM had 88% (95% CI, 0.73-1.0) Sensitivity in patients with Dementia (p=0.0027) which is higher than the overall BCAM sensitivity. BCAM also had modest performance in patients with poor baseline cognitive performance as evidenced by Short Portable Mental Status Questionnaire (SPMSQ).
Conclusions: This is the first study evaluating the BCAM in General medicine inpatient unit. Prior studies have validated BCAM in ED population. In our study, BCAM showed moderate sensitivity and good specificity for detecting delirium. BCAM had higher sensitivity in patients with dementia. From our study we conclude that BCAM when performed by bedside nursing staff improves delirium detection rate. However, to improve the diagnostic accuracy and the sensitivity it needs to be applied by trained clinicians.