Background: Febrile infants under 60 days-old undergo extensive evaluation for infection. Recent AAP guidelines recommend evaluation of the procalcitonin (PCT) level in the work-up of febrile infants 8-60 days-old to aid in predicting bacterial infection (BI) due to its high specificity; however, the sensitivity of PCT is relatively low. Recent literature has identified the Procalcitonin-To-Albumin (PCT:Alb) ratio as a means to predict bacterial infection in adults and this biomarker may have improved sensitivity over PCT alone. The objectives of this study are 1. To determine if a higher PCT:Alb ratio correlates with a positive bacterial culture in febrile infants. 2. To compare the sensitivity and specificity of the PCT:Alb ratio and PCT level to detect BI in febrile infants.
Methods: A retrospective cohort study examined infants 8-60 days-old presenting to a tertiary children’s hospital with fever between 1/1/2018-12/31/2020. Infants were identified via ICD-10 codes for fever or bacterial infection (bacteremia, meningitis, urinary tract infection). Exclusion criteria included prematurity (< 37 weeks), previous admission for infection or to intensive care, current or prior antibiotic use, or complex care needs. Data was collected for PCT and albumin levels, and bacterial cultures. Patients were considered to have a BI if they had a positive blood, urine, and/or cerebrospinal fluid (CSF) culture, if the treating clinicians documented the culture as true infection and not contamination, and if the infant received appropriate antibiotic treatment for the presumed infection. Logistic regression quantified association of BI with each PCT:Alb ratio and PCT levels using odds ratios (ORs). Predictive ability was estimated using the area under the curve (AUC) and corresponding sensitivity and specificity of PCT:Alb and PCT to detect BI.
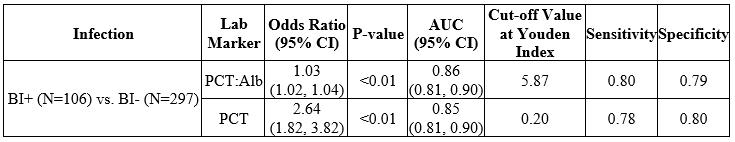
Results: Of the 403 infants meeting the inclusion criteria, 106 (26%) had a positive blood, urine, or cerebrospinal culture, and 297 (74%) were negative for BI. There was a statistically significant increase in the odds of having a BI with a higher PCT:Alb ratio (OR = 1.03, 95% CI [1.02, 1.04]; p< 0.01) and higher PCT level (OR = 2.64, 95% CI [1.82, 3.82]; p< 0.01) (Table 1). Based on AUC analysis using the maximum Youden Index, PCT:Alb ratio had a sensitivity of 80% and specificity of 79% (Youden Index = 0.59), and PCT had a sensitivity of 78% and specificity of 80% (Youden Index=0.58) (Table 1).
Conclusions: In febrile infants aged 8-60 days, elevation of both the PCT:Alb ratio and PCT level were associated with a statistically significant increase in the odds of having a BI. The PCT:Alb ratio and PCT level also demonstrated similar sensitivities (80% vs. 78%) and specificities (79% vs. 80%). In conclusion, the PCT:Alb ratio is comparable to PCT as a predictor for BI in our febrile infants under 60 days-old population. Further multicenter studies with a larger infant population are recommended, as well as a focus on serious BI (bacteremia and meningitis).