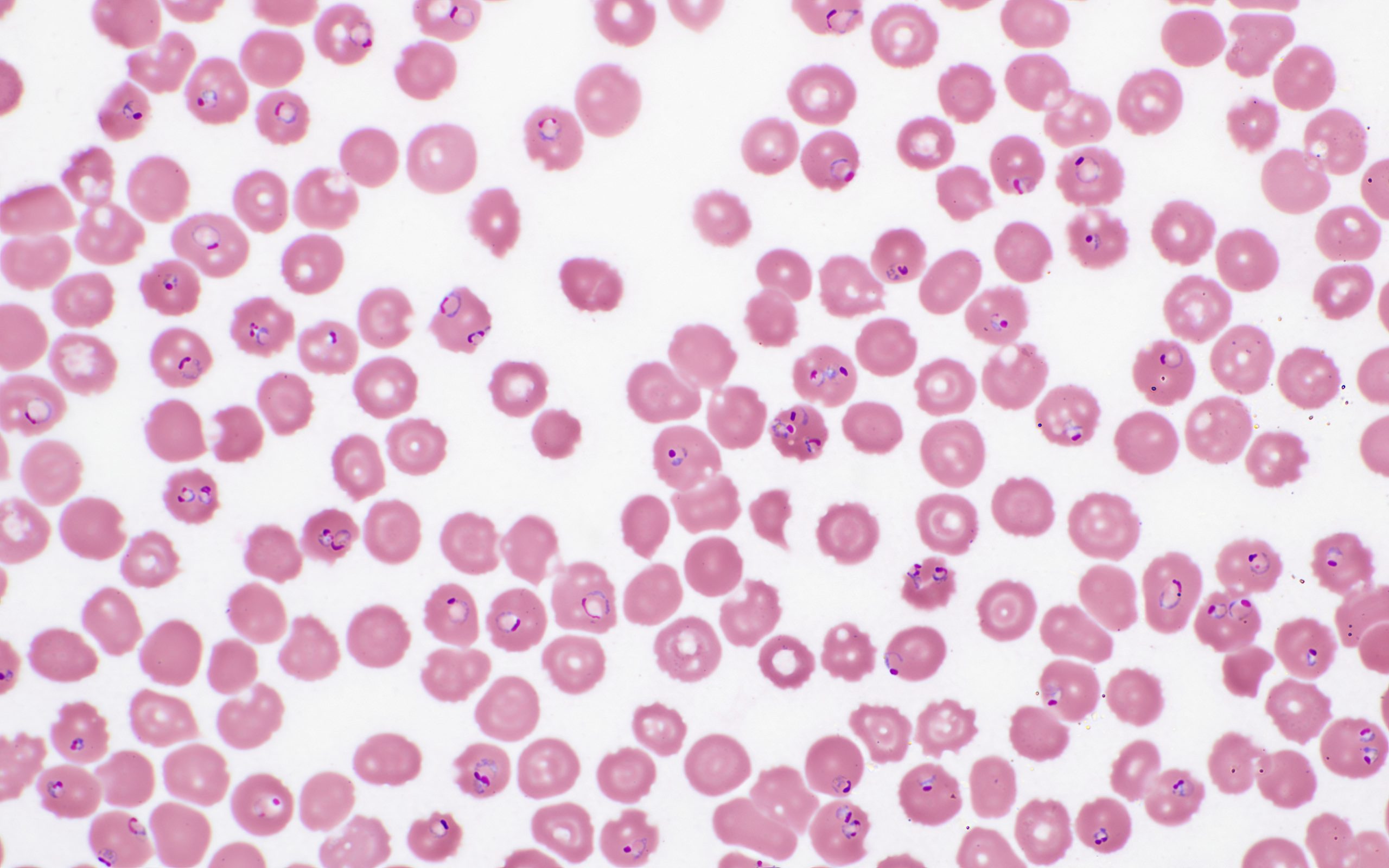
Case Presentation: A 25-year-old Wolof-speaking male who recently arrived from Senegal with remote history of malaria (unclear treatment, no hospitalization) presented to the hospital with a three-day history of dull global headache, abdominal pain, vomiting, watery diarrhea, and hematuria. Upon arrival, he was noted to be diaphoretic, dehydrated, tachycardic, and hypoglycemic. Labs were significant for severe thrombocytopenia, lactic acidosis, indirect hyperbilirubinemia, severe acute kidney injury (AKI), and parasite smear with 40% RBCs Plasmodium Falciparum. Given the considerable parasite burden and his high risk for rapid decompensation, he was admitted under medicine with critical care and infectious disease consultants following closely. The patient received fluid resuscitation, platelet transfusion, and intravenous (IV) artesunate. After several hours, he became lethargic and minimally responsive, febrile to 104.1F, hypoxic, and found to be acutely anemic with a hemoglobin of 5.9. He was subsequently admitted to the intensive care unit (ICU) for severe malaria with a guarded prognosis. In the ICU, following the completion of two doses of IV artesunate, the patient had rapid improvement of clinical course including resolution of fever, AKI, mentation, thrombocytopenia, and concurrently, reduced parasite burden to 11.2%. Chest X-ray, CT head, US abdomen, EEG, and eye exam were negative. He was transitioned to oral artemether-lumefantrine for three days. Repeat parasite smear showed no parasitemia and he was discharged home.
Discussion: Malaria is a potentially serious and life-threatening mosquito-borne infectious disease caused by Plasmodium parasites, which affects red blood cells. Plasmodium falciparum remains the most dangerous species, responsible for the most severe cases and deaths. Less than one percent of cases are classified as severe malaria, defined as acute malaria with signs of organ dysfunction, in the setting of hyperparasitemia. Such signs are the result of parasitized red blood cells adhering to the endothelial cells lining small blood vessels causing small infarcts, capillary leakage, and massive intravascular hemolysis. This clinical vignette illustrates the potential of severe malaria to progress rapidly to life-threatening multiple organ dysfunction, in this case within hours of presentation he became unresponsive and hypoxic, and concurrently the very quick response to Artemisinin-based combination therapy (ACT), in this case, clearance of parasitemia within 24-72 hours of ACT initiation. Recognition of the importance of frequent clinical and laboratory assessments, in this case, he was screened into the ICU, and prompt treatment, in this case, the infectious disease team coordinated ACT initiation, is imperative in mitigating the high mortality associated with severe malaria.
Conclusions: This case presents a compelling case of a young male with a remote history of malaria, who experienced a complex clinical course. His condition was characterized by a florid progression to encephalopathy and acute hypoxic respiratory failure, compounded by acute anemia and severe thrombocytopenia. The patient’s clinical course rapidly deteriorated, leading to shock necessitating ICU admission. This case underscores the need for heightened awareness and vigilance in diagnosing and managing severe malaria, particularly relevant in West Harlem, New York City, with the relevant epidemiological exposure within the large West African communities.