Background: Assessing vitals at regular intervals can be disruptive to a patient’s rest and unnecessary if the patient is clinically stable. These interruptions may lead to impaired sleep, parental fatigue and anxiety, delayed discharge, and increased cost of care. Moreover, alarm fatigue has been described with over-monitoring of patients, as has the overuse of staff resources that might be better utilized in other patient care activities. At our tertiary freestanding children’s hospital, we found that clinically stable patients received 5.9 interruptions/24 hours related to obtaining heart rate, respiratory rate, blood pressure, and temperature measurements every 4 hours per policy. Importantly, the recorded vital signs were almost always within normal ranges and did not change the patient’s medical management.Purpose: To reduce unnecessary interruptions to 2 per 24 hours in clinically stable patients
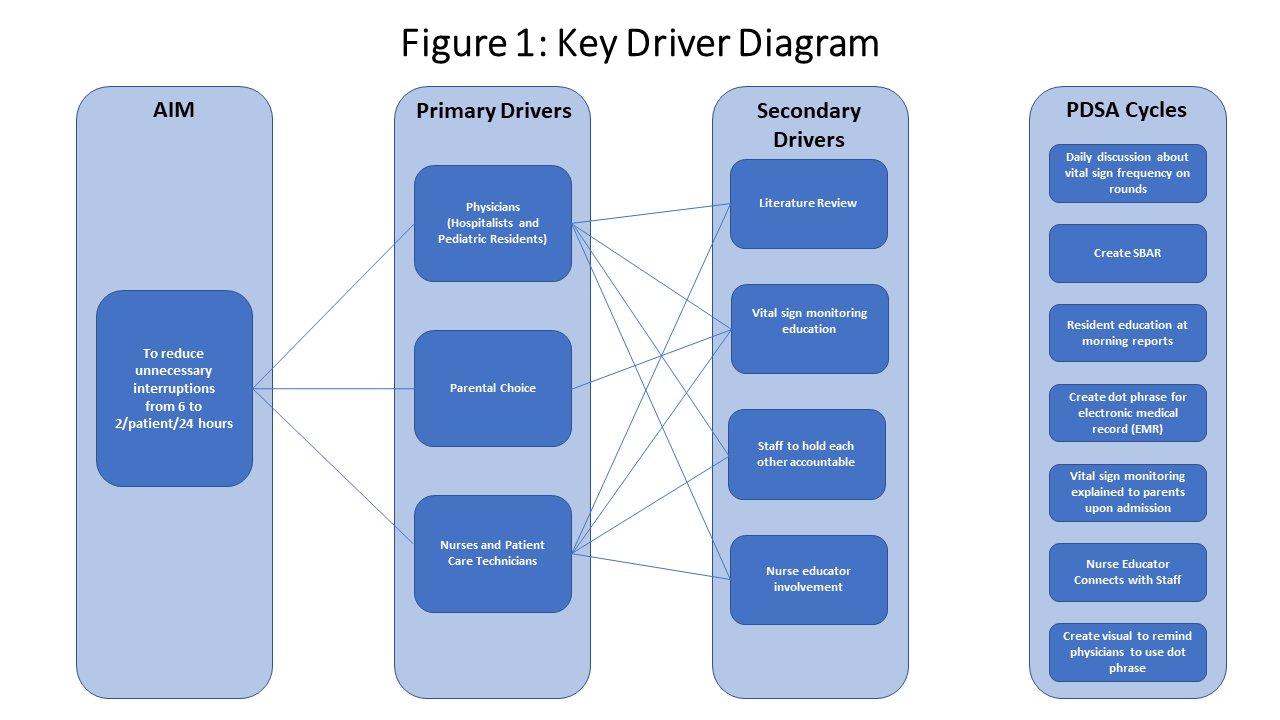
Methods: A team consisting of attending physicians, fellows, residents, and nurses defined “unnecessary interruptions” as blood pressure and temperature measurements for patients who were clinically stable because obtaining these can be invasive and disruptive. Patients were determined to be clinically stable if they had two consecutive Pediatric Early Warning Signs (PEWS) scores of 0 – 2 and in the green zone, did not require supplemental oxygen or require continuous monitoring per policy. We worked with an improvement specialist to reach our aim and create interventions (Figure 1). We piloted this project on one floor of a tertiary freestanding children’s hospital and only included patients admitted to the hospitalist service. Our interventions to decrease invasive vital sign frequency included (1) nursing education, (2) daily discussions about vital sign frequency on rounds, (3) creating a dot phrase for residents to more easily enter the order for reduced vitals, (4) education at resident morning report, and (5) creating visual reminders for the residents. We also created an infographic for parents to help them understand what PEWS scores meant and how we were monitoring their child’s vitals.
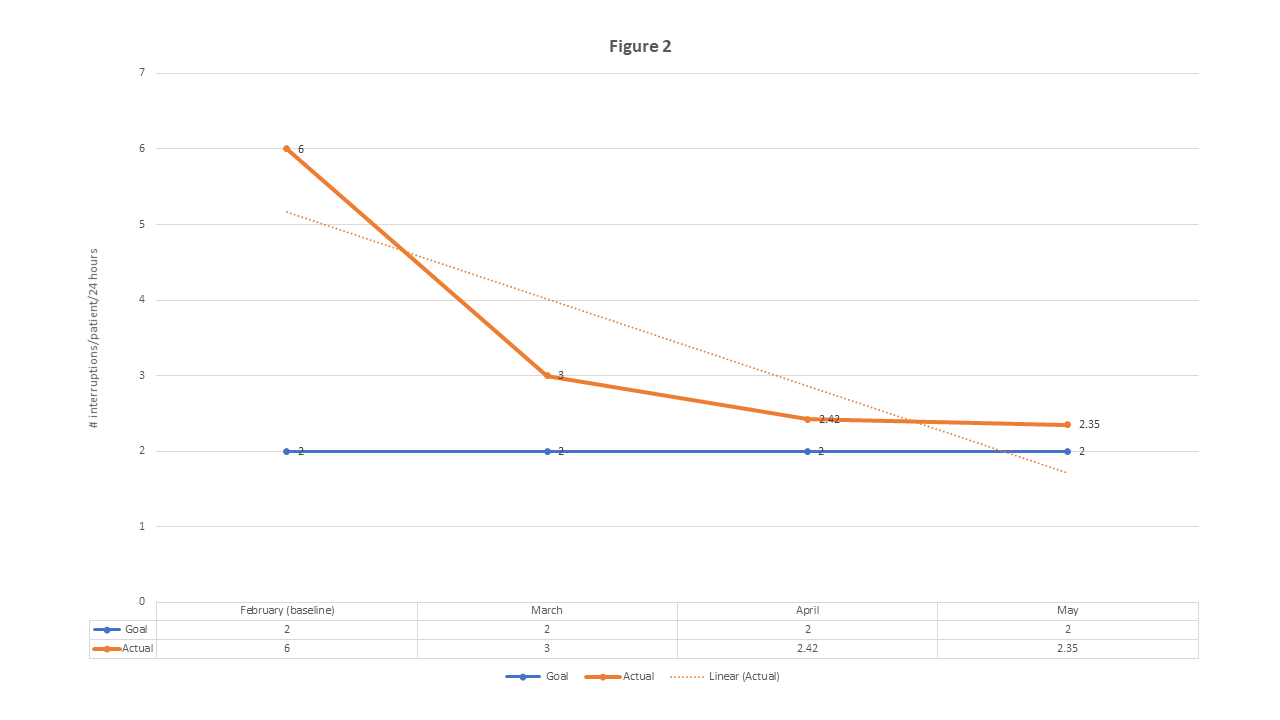
Results: Interruptions decreased from 5.9 to 3/patient/24 hours by 30 days after implementing our interventions; dot phrase adherence was only 67% at that time. To improve adherence rates, we created posted signs on the rounding computers to remind residents to enter the dot phrase. At 60 days, dot phrase adherence increased to 73% and interruptions decreased to 2.4/patient/24 hours. At 90 days, dot phrase adherence increased to 81% and interruptions decreased to 2.35/patient/24 hours (Figure 2). No critically ill or deteriorating patients were missed despite the reduction in blood pressure and temperature assessing frequency.
Conclusions: This multidisciplinary project incorporating nurses, hospitalists, and residents was able to successfully and safely decrease unnecessary interruptions using Pediatric Early Warning Scores as an indicator of clinical stability. Educating nurses, residents, and families about the benefits of reducing unnecessary interruptions was vital to the acceptance of this intervention. This project was well received by nurses, patient care technicians, residents, and parents. Additionally, the effects have been sustainable and applicable to other general pediatric inpatient units and should be considered safe.