Background: The value of follow-up blood cultures (FUBCs) to document clearance of bacteremia due to gram-negative bacilli (GNB) has not been well-established. Although previous studies suggested the yield of FUBC for GNB bacteremia is low, it remains to be elucidated for whom FUBC may be beneficial and for whom unnecessary. The objective of the study is to identify risk factors for persistent GNB bacteremia and to better guide clinicians’ decisions as to which patients may or may not benefit from FUBC.
Methods: A retrospective cohort study was performed at 4 acute care hospitals. Participants included adult patients with GNB bacteremia who had FUBC and were admitted between January 2017 and December 2018. Patients were excluded if they were younger than 18 years of age or if the initial positive blood culture was considered contamination by treating medical providers. We performed a multivariate logistic regression analysis to identify risk factors for persistent GNB bacteremia. Age, gender, and patient characteristics that were significantly associated with positive FUBC in univariate analysis were examined for correlation prior to inclusion in the multivariate analysis. Finally, we calculated the yield of FUBCs by dividing the number of cases found to have positive FUBCs by the number of total episodes of GNB bacteremia that had FUBCs performed. We identified the yields of FUBCs in all patients with FUBCs, and compared the yields in patients with or without any of the independent risk factors which were identified in the multivariate analysis.
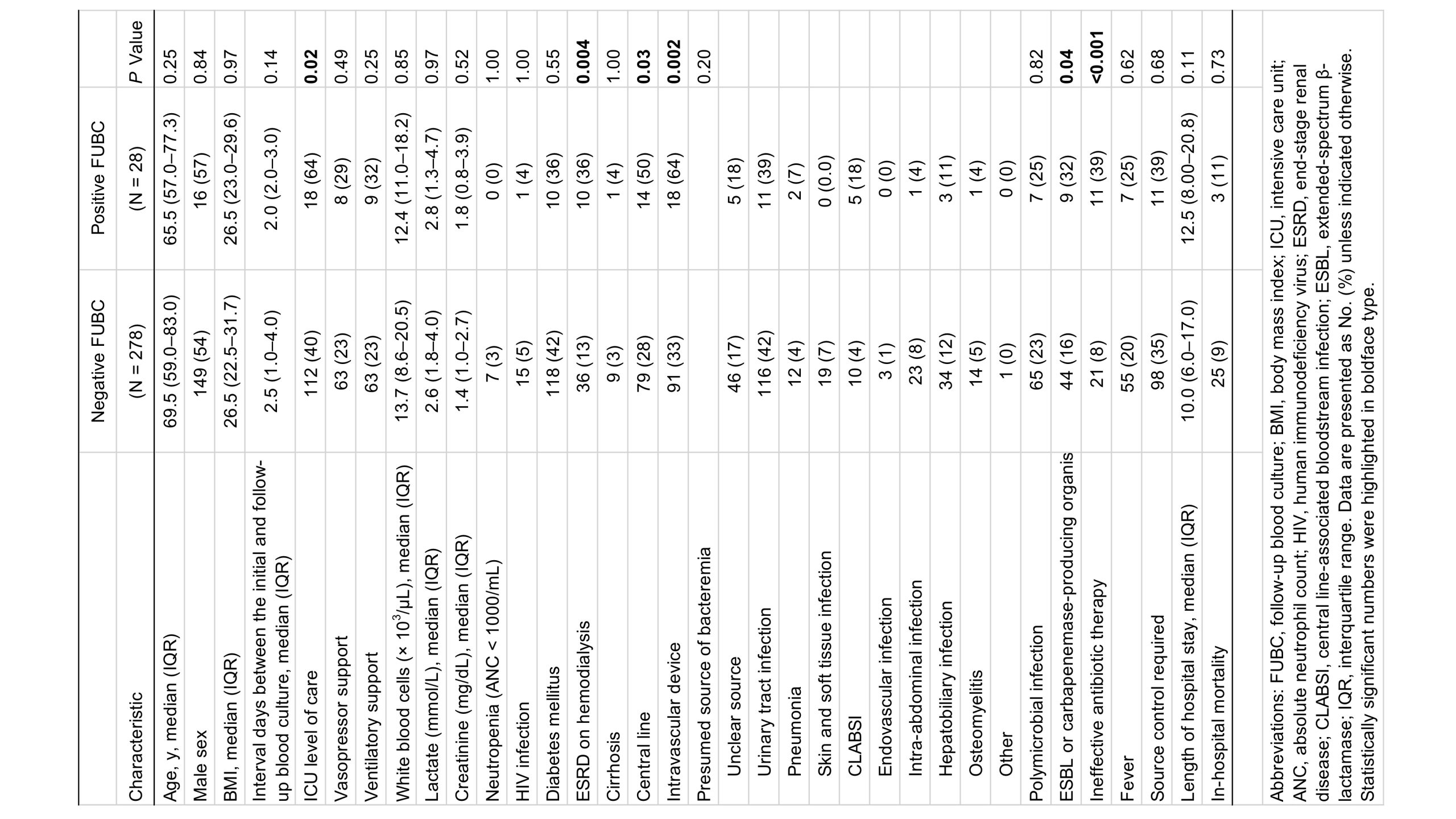
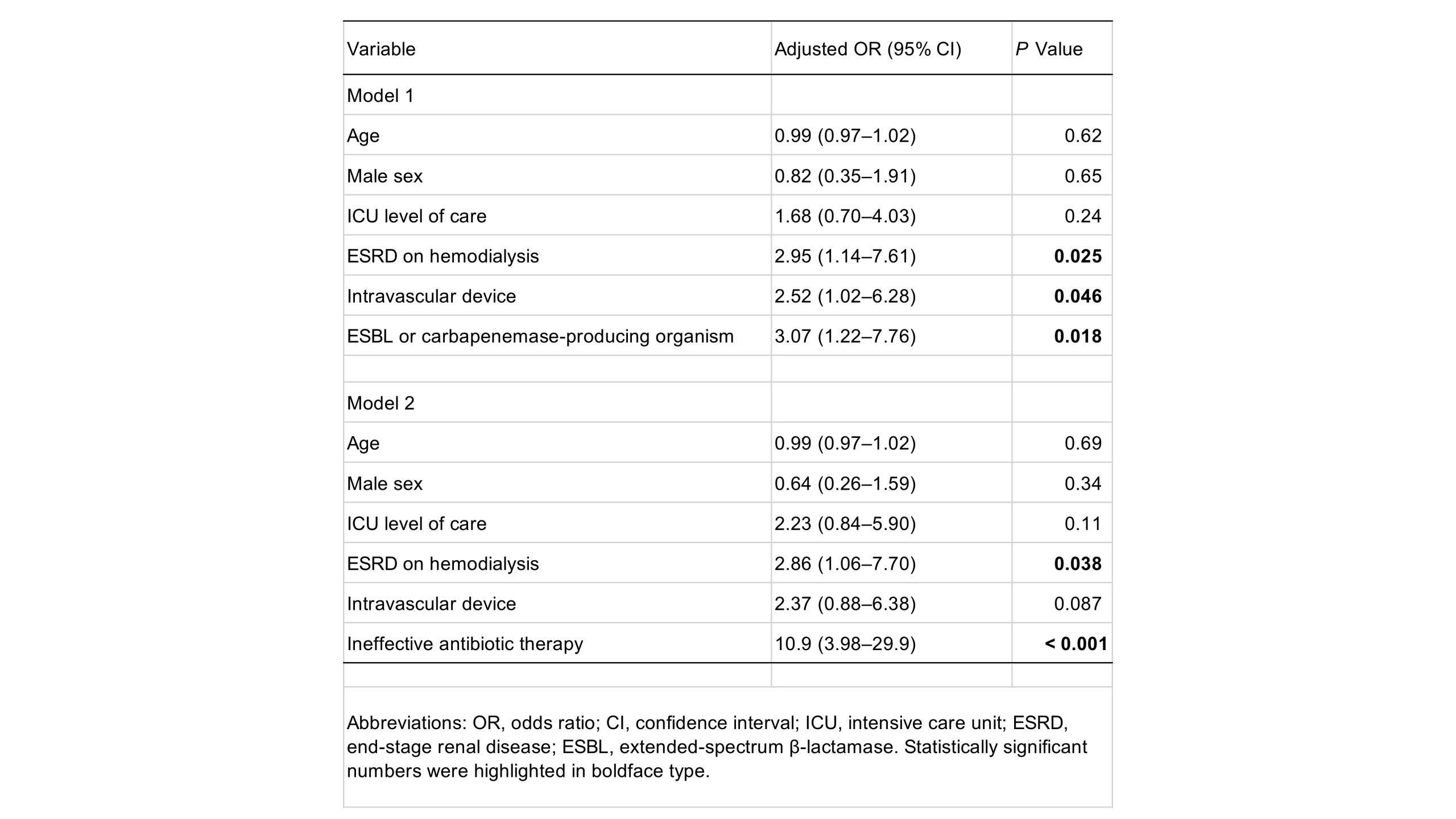
Results: There were a total of 463 patients with blood cultures which grew GNB during the study period. Of 306 patients with GNB bacteremia who had FUBC, 9.2% had persistent bacteremia. Patients with persistent GNB bacteremia were significantly more likely to be in the ICU (64% vs. 40%, P = 0.02), have ESRD on hemodialysis (36% vs. 13%, P = 0.004), central line (50% vs. 28%, P = 0.03) and intravascular device (64% vs. 33%, P = 0.002) as comorbidities, have ESBL or carbapenemase-producing organisms as the cause of bacteremia (32% vs. 16%, P = 0.04), and receive ineffective antibiotic therapy (39% vs. 8%, P < 0.001), compared with patients with negative FUBC (Table 1). In the multivariate logistic regression analyses, ESRD on hemodialysis, intravascular device, and either bacteremia due to ESBL or carbapenemase-producing organism or ineffective antibiotic therapy were identified as independent predictors for persistent GNB bacteremia (Table 2). 4-7 FUBCs and 23-30 FUBCs were needed for patients with ≥1 or no risk factors, respectively, to yield 1 positive result.
Conclusions: While the yield of FUBC for GNB bacteremia in patients with the risk factors may be comparable to gram-positive cocci bacteremia, the yield was very low in patients without the risk factors. We may limit performing FUBC to patients with GNB bacteremia who have ≥1 risk factors.