Background: Hospital readmissions are an important marker of healthcare quality, reflecting worse patient outcomes and resulting in millions of dollars of penalties annually. Medication nonadherence is an important driver of hospital readmissions, with one significant factor being difficulty obtaining medications after discharge. The difficulty could be due to copays, availability, or transportation to a local pharmacy. Medication delivery before hospital discharge is a proposed solution. Evidence is lacking on the benefits of bedside medication delivery programs as well as providing a limited supply of free medications to patients who cannot pay to fill their prescriptions. To improve medication adherence and readmissions, this project implements and analyzes the results of a pre-discharge medication delivery program at a large urban academic hospital. We aim to reduce readmissions by 5% through filling medicines on discharge to home and providing free medicines for patients who cannot afford to fill their prescriptions over one year.
Methods: We implemented a multidisciplinary “Meds in Hand” program with the community pharmacy located in our hospital. The program included sending electronic prescriptions to the pharmacy before discharge, which patients could pick up at the downstairs pharmacy or have delivered to their rooms. In addition, we implemented a “Social Services” program which paid medication copays for under- or uninsured patients for 30 to 90 days using social services funds. We then compared 30-day readmissions for hospital medicine patients utilizing the Meds in Hand and Social Services programs and hospital medicine patients not utilizing the programs over one year. Secondary analysis included readmissions by diagnosis.
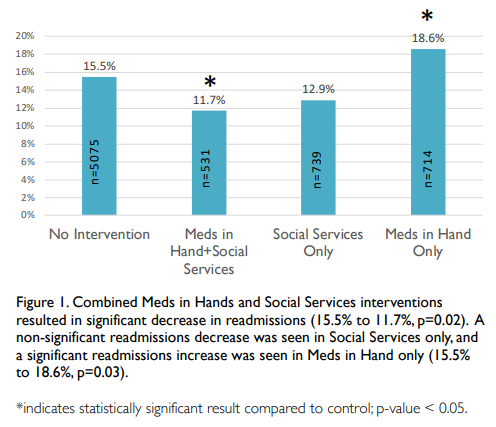
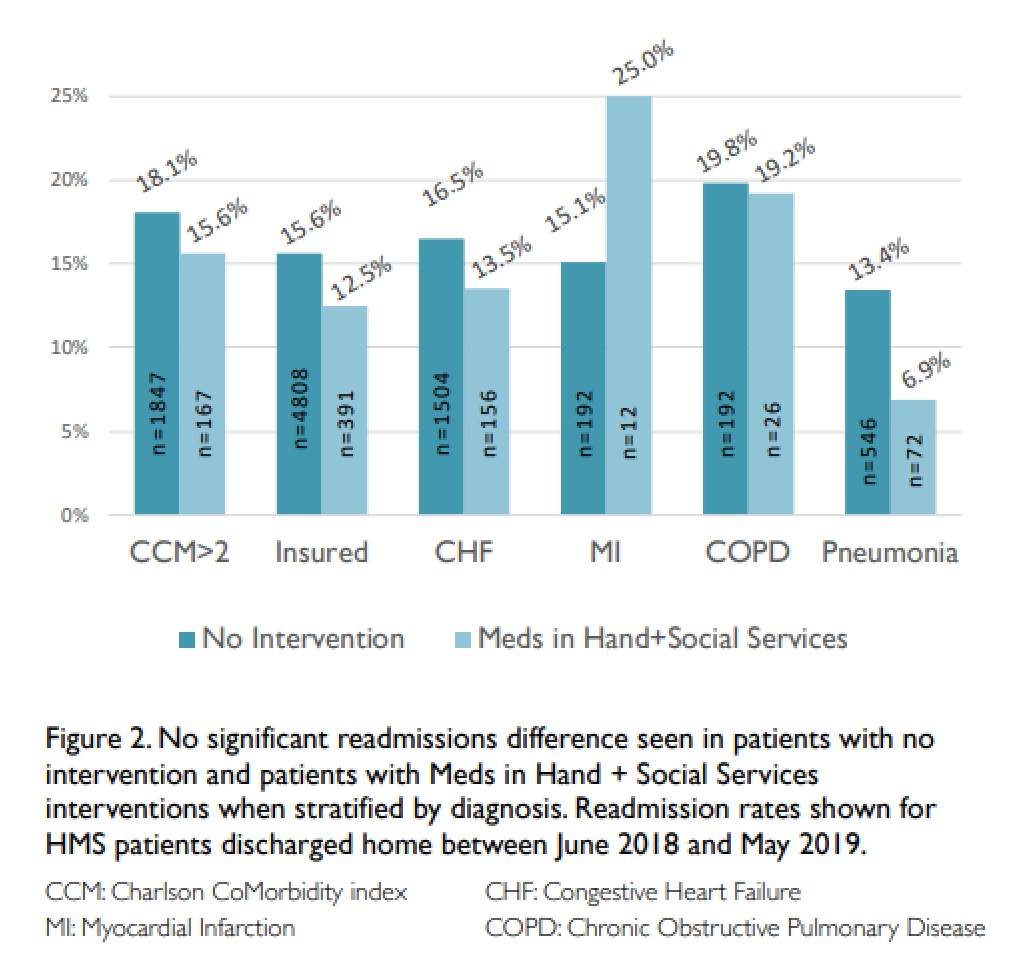
Results: Of 7059 HMS patients hospitalized between June 2018 and May 2019, 739 participated in Social Services program, 714 were in Meds in Hand program, and 531 participated in both. Thirty-day readmissions decreased from 15.5% for patients with no intervention to 11.7% for patients receiving both Meds in Hand and Social Services interventions (p=0.02). Thirty-day readmissions were 12.9% for patients in the Social Services program only (p=0.07 compared to patients with no intervention). Thirty-day readmissions significantly increased between patients with no intervention and patients in the Meds in Hands program only (15.5% to 18.6%, p=0.03). Secondary analysis by diagnosis showed non-significant differences in readmissions.
Conclusions: Among HMS patients, readmissions decreased significantly for patients who both had medications paid for and received medications before discharge. Readmissions showed a nonsignificant decrease for patients who only had medications paid for. Readmissions increased among patients who received medications before discharge but did not have medications paid for, likely due to nonrandomization. By providing medications before discharge, we helped remove a healthcare barrier and improved readmissions.