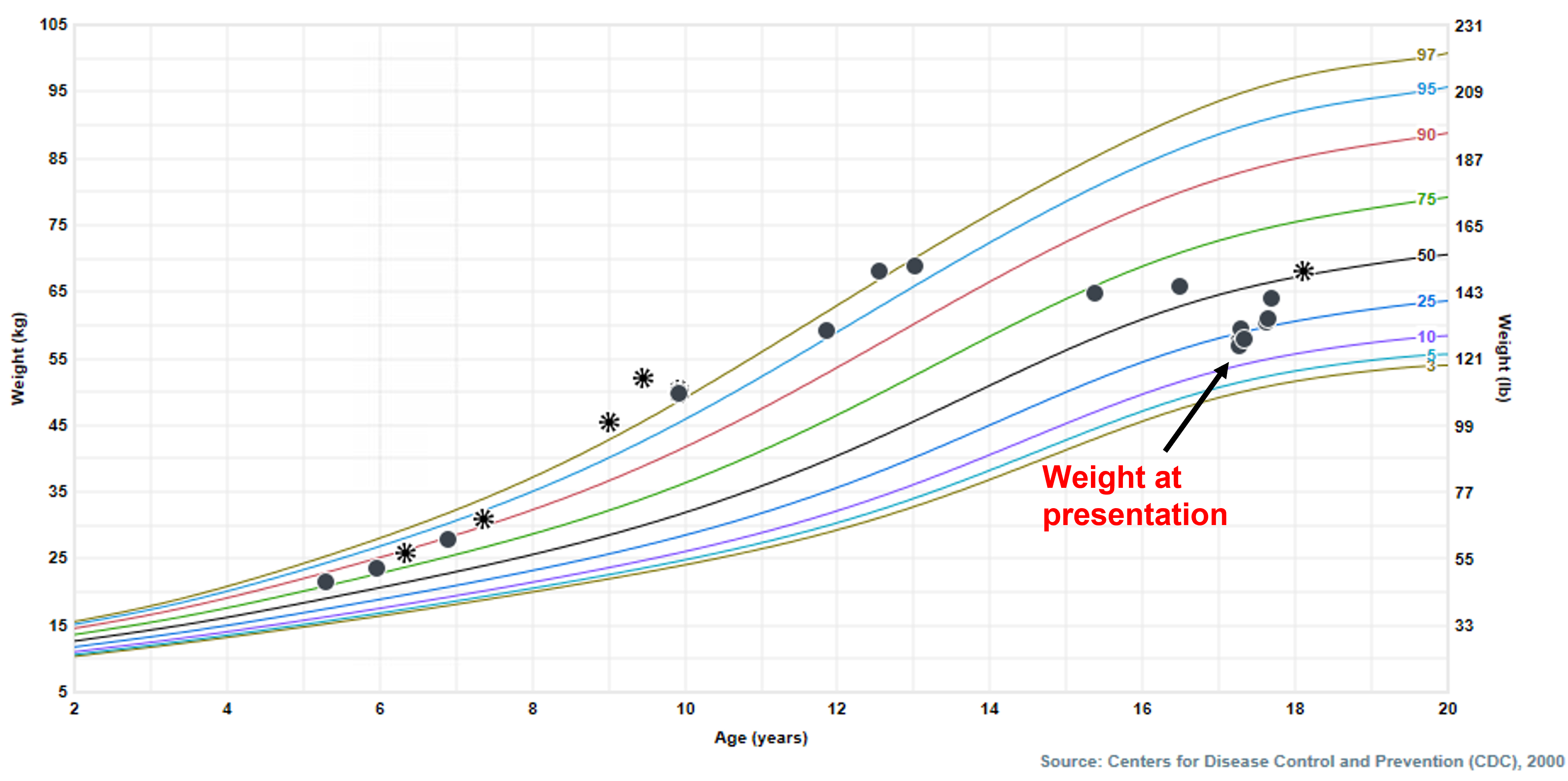
Case Presentation: A seventeen year-old male was admitted for two weeks of intractable nausea and vomiting in the setting of daily marijuana use over the last two years. Symptoms were associated with weight loss (9 kg over 2 weeks) and temporarily improved with frequent hot showers (Figure 1). Despite the use of commonly effective antiemetic medications such as droperidol, ondansetron, metoclopramide, and topical capsaicin, nausea and vomiting continued throughout the hospital stay with minimal relief. Initial labs were negative for pancreatitis, celiac disease, thyroid dysfunction, diabetes mellitus, and inflammatory bowel disease. Head and Abdomen CT and Esophagogastroduodenoscopy were unremarkable. He was eventually diagnosed with Cannabinoid Hyperemesis Syndrome (CHS) and started on total parenteral nutrition (TPN) due to poor oral intake. One week after admission, symptoms improved with the use of clonazepam which was started at 0.5 mg twice daily and titrated up to 1 mg twice daily. The patient was discharged after two weeks with a clonazepam taper. He followed up a week later with a complete resolution of symptoms, but has since been admitted twice and visited the emergency department several times due to the recurrence of symptoms with cannabis use.
Discussion: The rise in cannabis users and potency has led to the emergence of CHS within the pediatric population. CHS falls into the category of functional gastrointestinal disorders and presents with intractable vomiting, nausea, and abdominal pain in the setting of prolonged and excessive cannabis use (1). Resolution of vomiting episodes is achieved through sustained cessation of cannabis. A notable feature of CHS is a commonly seen pathological bathing behavior where the patient takes multiple hot baths and showers for symptomatic relief (2). Various mechanisms have been proposed to explain the etiology of CHS including genetic variations affecting the metabolism of cannabinoids, thermoregulatory dysfunction in the limbic system, and antagonism and/or downregulation of CB1 receptors in the endocannabinoid system, but no clear cause has been identified (2). The current literature review shows that standard antiemetics such as serotonin and dopamine antagonists are rarely effective in treating the symptoms associated with CHS (2). Reports with adult patients have found capsaicin cream, benzodiazepines, and haloperidol to have the best efficacy, however research in pediatrics is still scarce (3).
Conclusions: Pediatricians need to be familiar with CHS as an important cause of nausea, vomiting, and weight loss, particularly in the adolescent population. At this time, abstinence is the only known management strategy to prevent the recurrence of symptoms. Current research has shown multiple potentially effective treatment options in the management of the acute phase of illness, however, their true effectiveness and optimal dosing strategies remain unknown and require further investigation (4). Our case hopes to add to the growing literature on effective treatment strategies for CHS in the pediatric population.