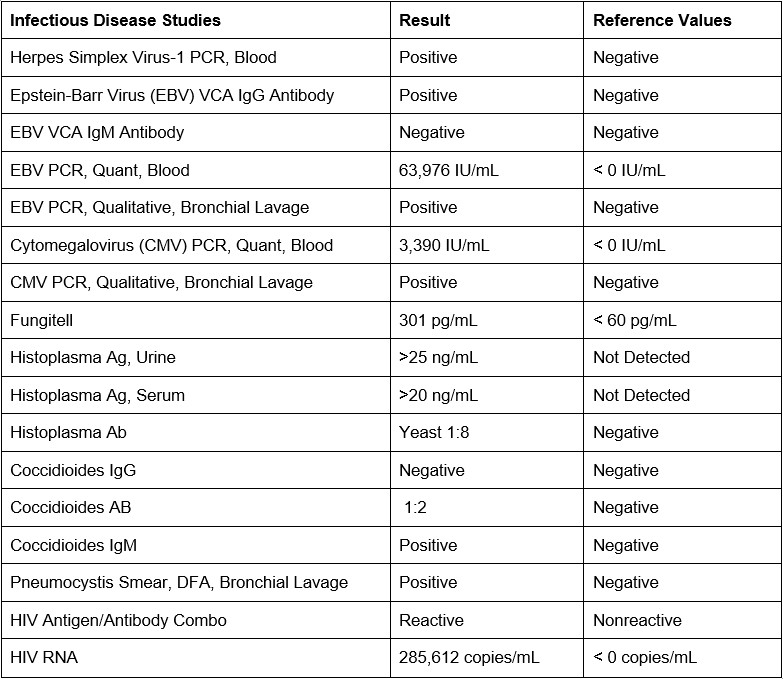
Case Presentation: An 18-year-old man presented with 2 weeks of fever, non-productive cough, and sore throat, as well as nausea, emesis, and unintentional weight loss of ~5kg. He was an undocumented immigrant but had not traveled outside of the country in the past 18 months and reported no sick contacts. He worked in landscaping but had no history of tick or insect bites. When interviewed by a Spanish speaking provider (rather than interpreter), he disclosed an insertive condomless vaginal sexual encounter less than 4 years prior. Physical Exam: Ill-appearing, thin male, lying in bed. He was febrile to 39.4C (102.9F) with a heart rate of 120 bpm and respiratory rate of 44. Oxygen saturation was >95% on ambient air. He had mild scattered petechiae in his oropharynx with crusted lesions present on his lips, as well as anterior cervical lymphadenopathy, hepatosplenomegaly, and delayed capillary refill. Diagnostic Evaluation: Initial labs revealed pancytopenia with lymphopenia and mildly elevated liver enzymes. Peripheral blood smear and bone marrow biopsy were normal without blasts. Given pancytopenia, persistent fevers, splenomegaly, and ferritin of 10,833.9 ng/mL (normal < 307.3 ng/mL), additional studies were sent for hemophagocytic lymphohistiocytosis (HLH). Soluble IL-2 receptor was elevated at 3,260 U/ml, meeting HLH diagnostic criteria. While awaiting his IL-2 test, his HIV test and several concommitant infectious studies became positive (Table 1). CD4 count was < 10. Chest CT showed bilateral diffuse punctate nodular opacities in a miliary pattern (Fig 1). Expectorated and lavaged AFB cultures were negative for TB and NTB, and the miliary pattern was attributed to histoplasmosis v pneumocystis.Diagnoses: HLH and HIV/AIDS complicated by HSV, EBV, CMV, PJP, coccidioides, and histoplasma co-infections.
Discussion: New diagnoses of advanced HIV should prompt a broad workup for concomitant opportunistic infections. HLH is an aggressive and maladaptive immune response that can present in response to those infections. Recognition allows appropriate treatment of those infections before adding antiretroviral therapy for HIV, as well as avoidance of the chemotherapy and immune modulators typically used for HLH. This patient was treated with acyclovir, trimethoprim-sulfamethoxazole, and amphotericin before ART therapy. No specific treatment for HLH was needed.The mechanism for how this patient contracted HIV was not determined. He disclosed a history of unprotected sex less than 4 years prior to presentation, which suggests an unusually rapid progression to AIDS. It is also possible he had prior exposures he was hesitant to disclose, or that he was exposed via mother to child transmission given his age and advanced disease at presentation. It is important to emphasize that this patient is an undocumented individual with low health literacy and is Spanish speaking. These factors likely created barriers, contributing to late presentation and advanced disease; in order to holistically and successfully treat him, these factors necessitate targeted, longitudinal support.
Conclusions: New diagnoses of advanced HIV should trigger a broad workup for concomitant opportunistic infections, and HLH can be present in those experiencing significant inflammatory burden.