Background: The 2016 State of Hospital Medicine report showed that the average hospitalist compensation model is composed of 80% base pay, 15% productivity, and 5% performance. Much variation exists by region in the make-up of the performance component with a rise in measures focused on patient satisfaction and readmission and significant differences in weight given to citizenship measures. It remains unknown whether a performance-based incentive can motivate academic hospitalists to provide high quality, high volume care while contributing to their group’s academic mission.
Purpose: We describe an incentive compensation (IC) model at an academic medical center that accounts for clinical excellence through productivity and adherence to quality measures and academic excellence through hospitalists’ involvement in education, research, and quality improvement.
Description: The prior IC model for our division was based on productivity plus incentives at the discretion of the chief. This model did not account for quality of work or academic contributions and the subjective nature of IC determination was a dissatisfier for faculty. To improve transparency and emphasize high quality care and contribution to the academic mission, we convened a task force in 2013 to revamp the method of determining IC. Our model now rewards 8-12% base pay determined by a point system for productivity, quality metrics, and academic work. Productivity points range from 1-5 with number of points awarded based on hospitalists’ total RVUs relative to their peers. Quality metric points also range from 1-5 with 2 points for professionalism and 1 point each for meeting attendance, prompt discharge summary completion, and consistent completion of discharge medication reconciliation. Finally, a maximum 5 points can be earned through academic activities that mirror those required for maintenance of academic appointments at our institution. Points in the three categories are totaled and IC is determined by the quintile in which the individual falls.
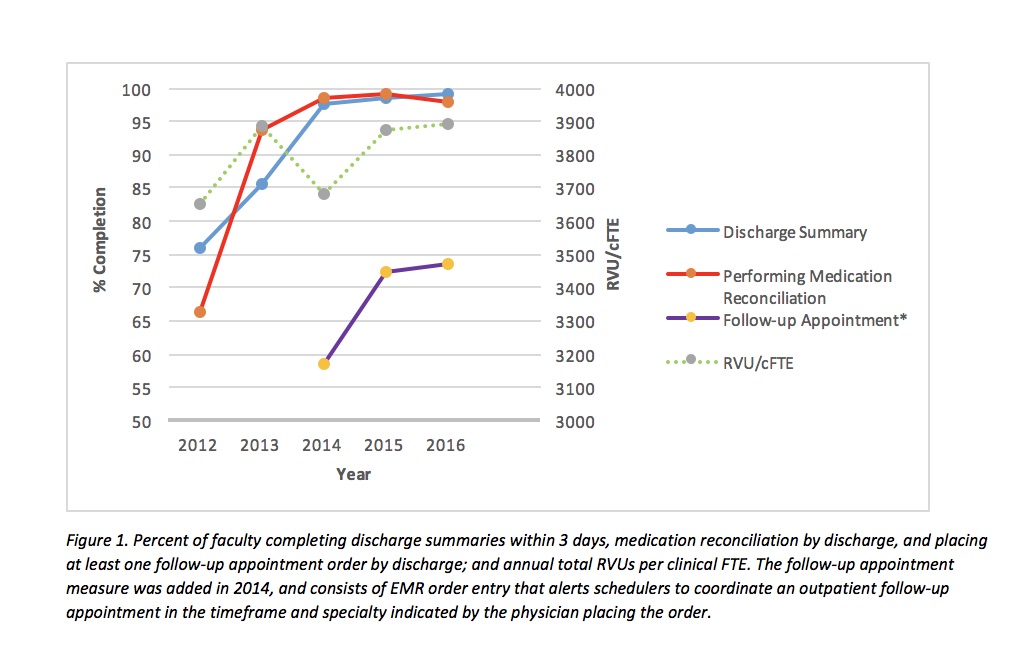
After implementation of this model, discharge summary completion improved from 76% to 99% and medication reconciliation from 66% to 99% between 2012 and 2015. RVU differences among providers remain minimal but hospitalists who see more patients on admitting shifts or volunteer for moonlighting shifts tend to fall in the higher quintile. We have seen a moderate increase in academic achievements since the implementation of the IC model including a greater percentage of higher academic rankings and a greater number of publications, conference presentations, and hospitalist-led quality improvement projects.
Conclusions: An IC model that rewards quality of care and non-clinical contributions can impact the delivery of care and further the academic mission of an academic hospital medicine group.