Background: Systemic Sclerosis (SSc) is an autoimmune condition characterized by widespread skin fibrosis and/or end-organ damage. Previous studies have reported variable outcomes of the disease process, with males and patients of certain ethnicities suffering from the severe form of the disease leading to end-organ damage and an increase in mortality (1,2). The aim of this study was to assess the outcomes of patients admitted with a known diagnosis of SSc. The primary outcome was incidence of acute coronary syndrome (ACS). Secondary outcomes included gender, race, intervention for ACS, development of acute kidney injury (AKI), and all-cause-in hospital mortality in patients with SSc.
Methods: In this retrospective analysis, we queried data from the National Inpatient Sample (NIS) for the years 2012-2019. We identified all patients (≥18 years of age) who had a discharge diagnosis of Systemic Sclerosis (n =52500) using their respective ICD-9 and ICD-10 codes. Among these patients, we identified those with an admitting diagnosis of acute coronary syndrome based on the relevant ICD codes. We further grouped patients based on gender and analyzed them for gender and race differences in outcomes including mortality; requirements for PCI/CABG, mechanical ventilation, vasopressors and hemodialysis; and development of AKI. Categorical variables were summarized as percentages and continuous variables were presented as mean±SD. Identification of risk factors was done using logistic regression models with inverse probability weighting for complex survey data. The univariate and multivariable association of presumed risk factors for mortality in Scleroderma patients with ACS was performed by a Cox proportional hazards model censored at length of stay.
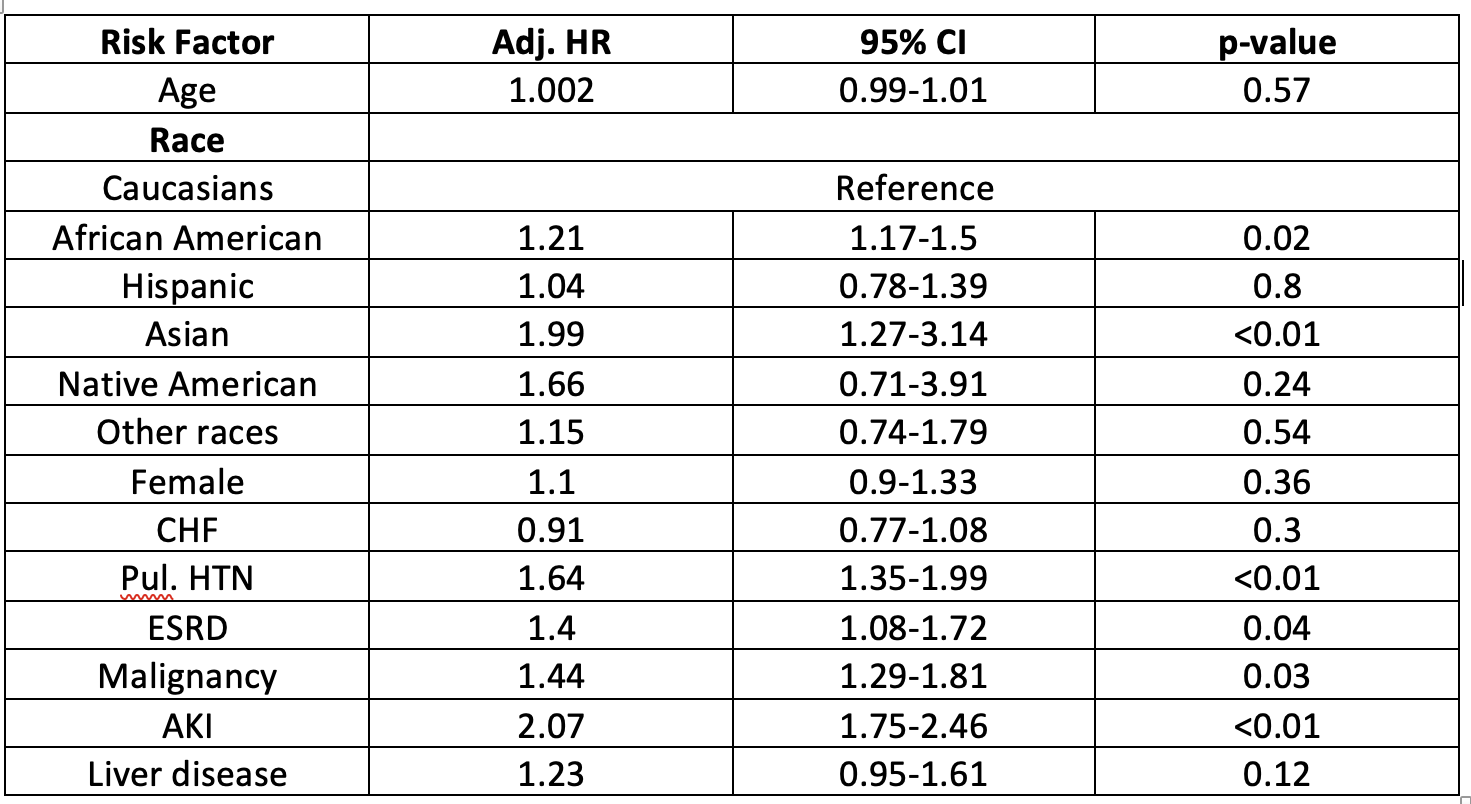
Results: Out of more than 7 million discharges from 2012-2019, 52500 patients with SSc were identified with males constituting 16% and females constituting 84%. A total of 7553 patients had an admitting diagnosis of ACS. Among all SSc patients, incidence of ACS was significantly higher among males as compared to females (19.98% vs 13.33%, p< 0.01). Caucasians had the highest incidence of ACS, followed by Asians (p< 0.01) while African Americans underwent PCI less than other racial groups (p< 0.01). Among SSc patients with ACS, Asians (adj. HR 1.99; 95% CI 1.27-3.14; p< 0.01) were at highest risk of mortality followed by African Americans (adj. HR 1.21; 95% CI 1.17-1.5; p=0.02) when compared to Caucasians (Table 1). Pulmonary hypertension (adj. HR 1.64; 95% CI 1.35-1.99; p< 0.01), ESRD (adj. HR 1.4; 95% CI 1.08-1.72; p=0.04), presence of malignancy (adj. HR 1.44; 95% CI 1.29-1.81; p=0.03) and development of AKI (adj. HR 2.07; 95% CI 1.75-2.46; p< 0.01) were associated with significantly higher risk of mortality (Table 1).
Conclusions: Our results indicate that the incidence of ACS in patients with SSc is correlated with gender and race, with males and Caucasians having the highest incidence. Asians and African Americans with SSc who get admitted for ACS have the highest risk of in-hospital mortality, demonstrating a racial disparity in the outcomes of these patients.