Background: Traditional review approaches to inpatient mortality remain flawed. M&M conferences, administrative data analysis, and chart review do not effectively leverage the frontline perspective, are frequently delayed, and may be perceived as punitive if not peer review protected.
Purpose: We developed an electronic mortality review tool that would: (1) permit rapid review of all inpatient deaths, (2) engage frontline clinicians, (3) require minimal time to complete, (4) be completed within 48-72 hours of inpatient demise, (5) allow data aggregation and trending across departments, and (6) facilitate rapid referral of cases requiring additional review and further action. We anticipated that this could more quickly identify the small fraction of truly preventable deaths needing further attention.
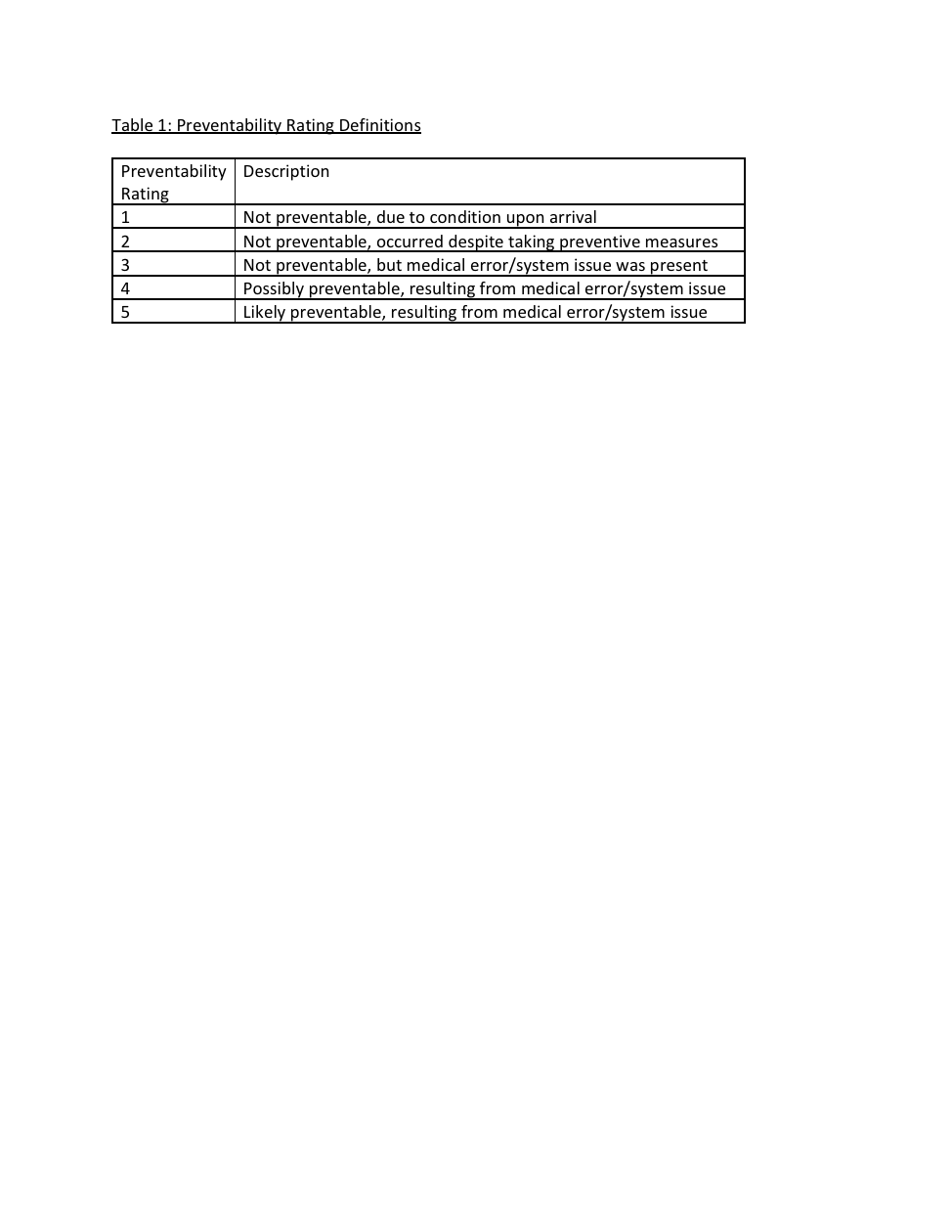
Description: We built an electronic, web-based data platform and electronic, web-based mortality review survey. The platform was integrated into our hospital’s electronic M&M platform through which all services review cases. We piloted the new mortality review process on four inpatient services on which the majority of inpatient deaths take place: hospital medicine, liver transplant, cardiology, and general surgery. Attending physicians and residents involved in the patient’s care at the time of death received an automated email with a link to a confidential, and peer-review protected survey asking about factors possibly contributing to the death, such as: complications, care delays, supervision, communication, and end-of-life issues. Respondents shared a short clinical summary, opinion on preventability (Table 1), improvement suggestions, and need for referral to risk management or for further review and action. We formed a working group of multidisciplinary providers, trainees, and nurses to review the pilot progress, provide feedback on both the electronic platform and review process, and follow up on referred cases. We tracked response rate, time to review and case closure, preventable deaths, and opportunities for improving care. Recognizing that deaths take an emotional toll, we invited providers to receive support from the hospital’s Caring for the Caregiver program.
From May 1-October 31, 2018, there were 169 deaths (75.8%) on hospital medicine out of 223 deaths across all four pilot services. On hospital medicine, the response rate for reviewing deaths was 98%. Providers identified a range of contributing factors. Of provider-assigned preventability ratings, 111 deaths were rated 1 (65.7%), 45 rated 2 (26.6%), 5 rated 3 (2.96%), 5 rated 4 (2.96%), and none rated 5. Twenty-three (13.6%) were referred to hospital medicine’s case review process for further discussion. Major systems issues identified in these cases included prolonged emergency department boarding and communication gaps with transfers from outside institutions. These systems issues were tracked across all pilot services and escalated to hospital leadership.
Conclusions: This pilot process facilitated timely review of inpatient deaths and rapid identification of those involving errors or systems issues needing further review and action. The web-based approach allowed for easy data aggregation and theme identification across services. The response rate was high and providers were engaged in the process, frequently making suggestions for how to improve care for patients.