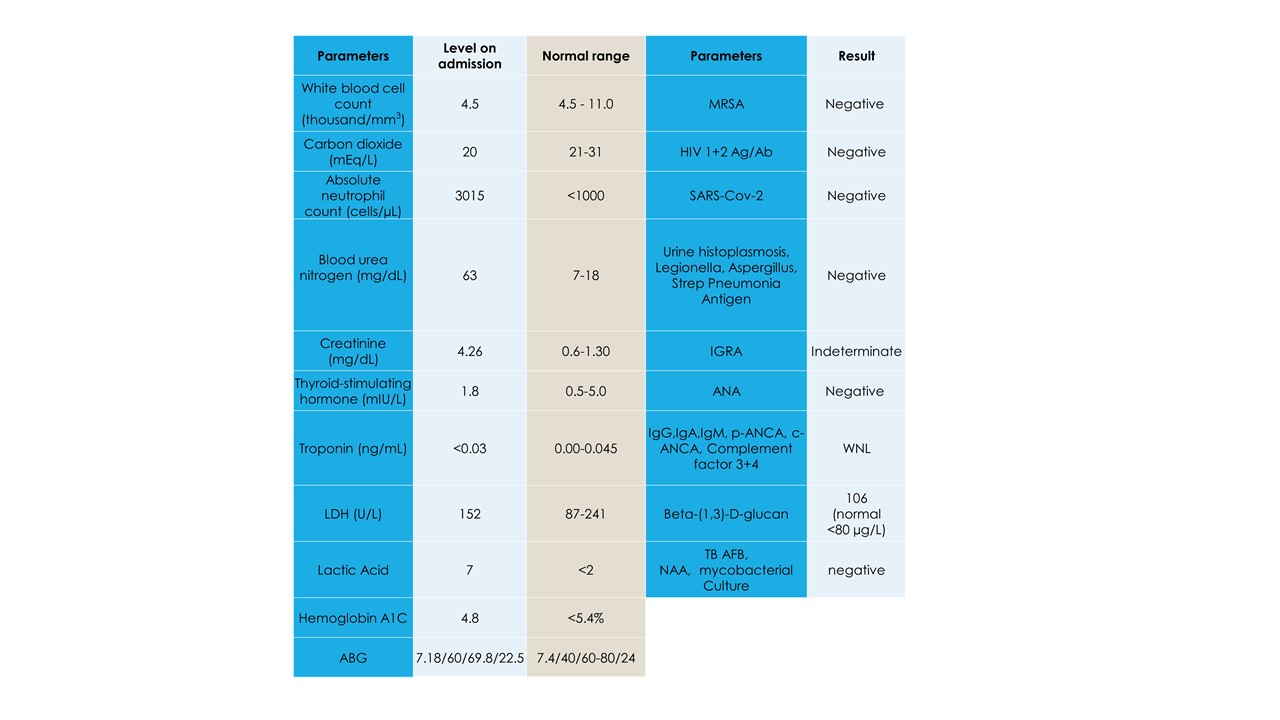
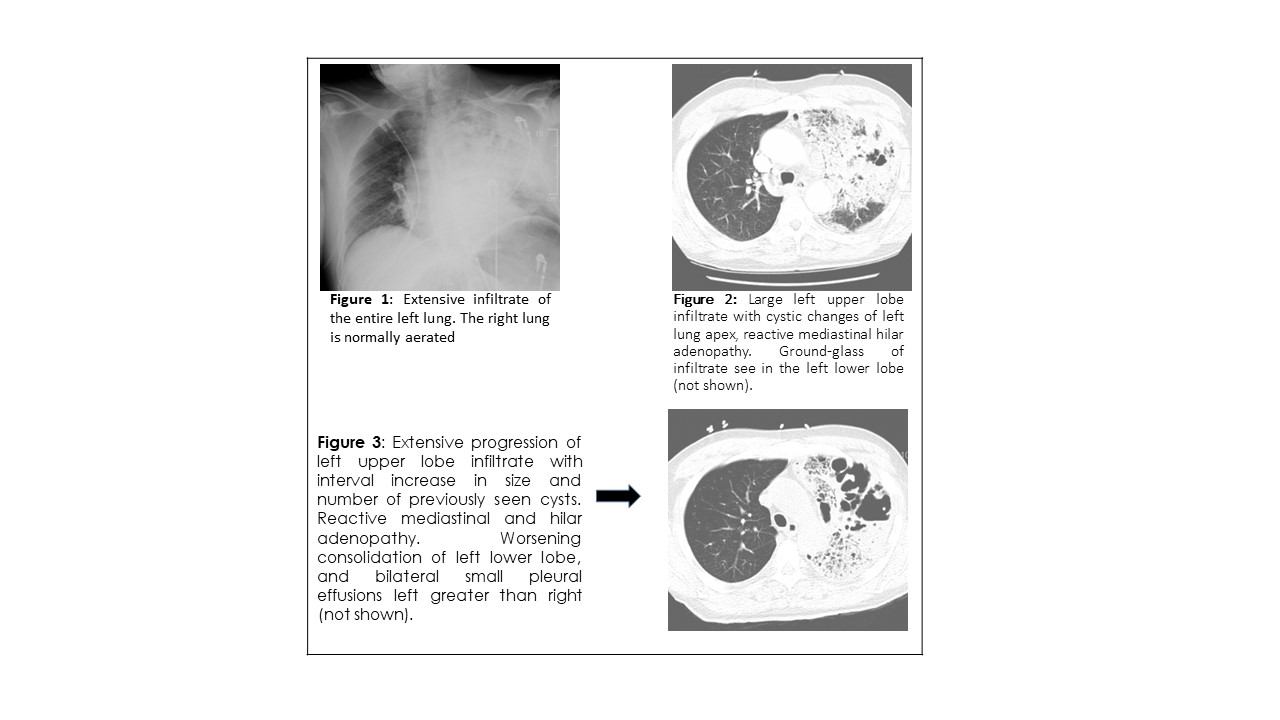
Case Presentation: A 61-year male presents with complaints of a cough and progressive dyspnea for over a week. Pertinent history included a Tuberculosis (TB) infection over thirty years ago with an unclear treatment course. Social history was positive for a 40 pack-year smoking history. On presentation, he was tachycardic, hypoxic and tachypneic. Physical exam was normal except for confusion and mild respiratory distress. Rales were audible in the left upper lobe. His admission workup can be found in Table 1. Imaging was consistent with a dense left upper lobe consolidation with cystic features concerning for cystic pneumonia (Figure 1),He was given a one-time dose of vancomycin, piperacillin and tazobactam, and doxycycline. Blood, sputum, and acid-fast bacilli (AFB) cultures were ordered, and respiratory droplet precautions were instituted.He was admitted to the ICU for severe sepsis secondary to cystic pneumonia, mixed metabolic and respiratory acidosis, acute hypoxic and hypercapnic respiratory failure, stage 3 acute kidney injury (AKI), and metabolic encephalopathy. Antibiotics were continued for cystic pneumonia, and intravenous fluids were administered for pre-renal AKI. Over the ensuing few days all acute conditions resolved, except for on going respiratory insufficiency, requiring 3L of oxygen. Left upper lobe infiltrate remained persistent on follow-up imaging (Figure 2), blood cultures were aseptic and AFB cultures were not obtained.Upon improvement the patient was then transferred to the medical floor where further TB workup including an interferon-gamma release assay (IGRA), and bronchoalveolar lavage (BAL) were ordered. On day 6, of isolation, bronchoscopy revealed thick, copious mucopurulent secretions from the left bronchus. TB testing was negative, and cultures grew Candida parapsilosis. He did not show improvement after completing ten days of antibiotics, hence further work up was pursued Table 1. A repeat CT showed progression of cystic pneumonia with an increase in size and frequency of cystic lesions (Figure 3).A repeat bronchoscopy was performed on day 12, and the results noted mild oropharyngeal thrush, left upper lobe irritation, and thick and copious secretions. Again, the BAL testing for TB was negative, while biopsies and cultures continued to show C. parapsilosis. On day 17, fluconazole was started, and the patient’s condition improved, along with a decrease in O2 support requirement. The patient was discharged with follow-up outpatient imaging recommended following one week of anti-fungal therapy.
Discussion: C. parapsilosis is an emerging fungal pathogen that has become an increasingly common cause of invasive fungal disease over the past few decades(3). A definitive diagnosis requires a biopsy for histopathology and is done only after exhausting all other common possibilities of pneumonia(5). C. parapsilosis infections are rare and pneumonia is not a typical manifestation of this Candidal species.It is postulated that C. parapsilosis pneumonia can occur in patients with chronic parenchymal lung damage from tobacco smoking. The infection may be triggered by trivial viral infections(7). In a case such us this one, involving worsening antibiotic resistant cystic pneumonia in an immunocompetent patient, it is important to keep in consideration unusual nonbacterial pathogens.
Conclusions: This case highlights the importance to consider unusual nonbacterial pathogens when treating antibiotic resistant pneumonia, even among immunocompetent patients.