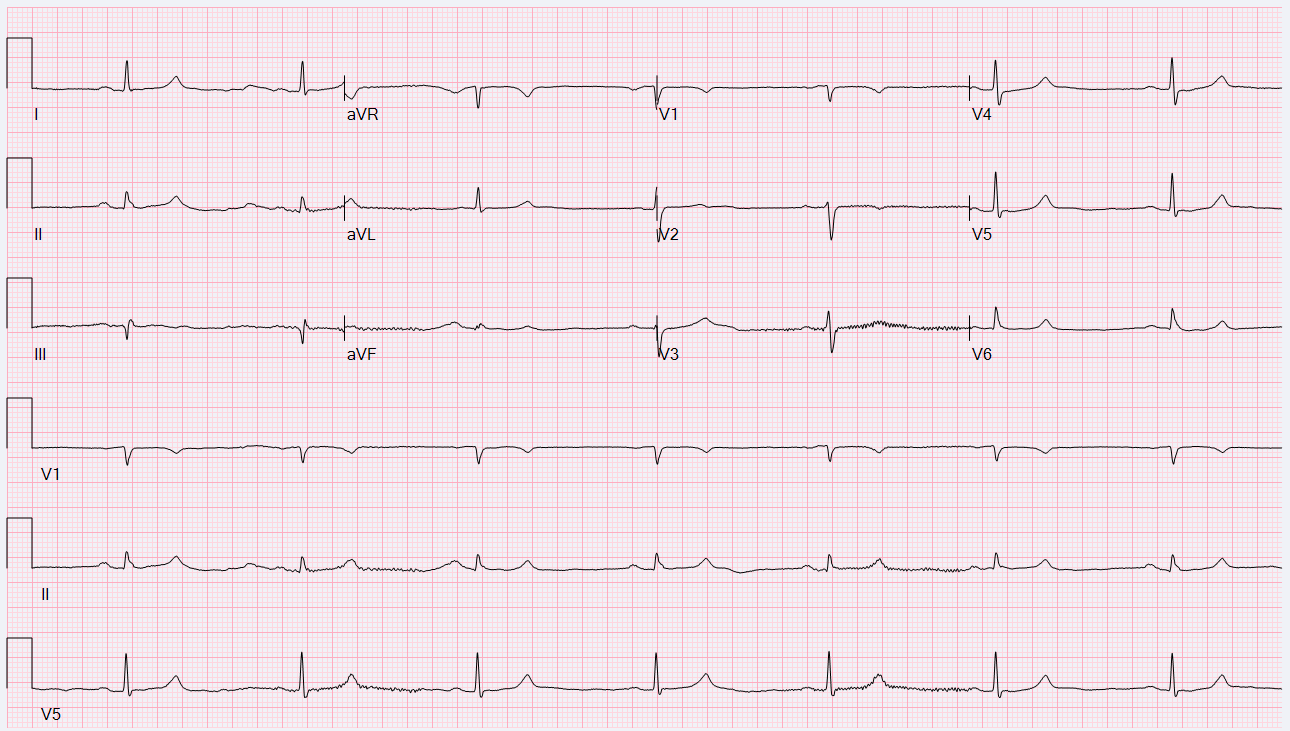
Case Presentation: A 57-year-old male with previous hemorrhagic stroke complicated by residual left sided deficits with vascular dementia, primary hypertension on a regimen of carvedilol 25mg twice daily, and recurrent urinary tract infections due to obstructive calculi presented with acute-onset lethargy and encephalopathy. Presenting vitals were notable for hypotension (64/53), bradycardia (43 beats per minute), and hypothermia (35.3 C). Physical exam demonstrated a somnolent and disorientated mental status as well as suprapubic tenderness. Laboratory studies confirmed the presence of hyperkalemia (6 mmol/L), azotemia (creatinine: 4.80 mg/dL and blood urea nitrogen: 53 mg/dL), hyperlactatemia (2.9 mmol/L), acidemia (pH of 7.21 on venous blood gas), leukocytosis (12,100 per uL), and bacteriuria (30,000 cfu/mL of Escherichia Coli) with pyuria (greater than 150 leukocytes per high-powered field). Electrocardiogram revealed marked sinus bradycardia. Chest and abdominal radiographs were without abnormality.The patient was promptly resuscitated with fluids and admitted to the intensive care unit for management of circulatory shock and hyperkalemia with epinephrine infusion and intravenous calcium and insulin. Antibiotics were empirically started for severe sepsis due to acute complicated urinary tract infection. He had subsequent hemodynamic and renal recovery and was transferred to the medical floor for continued management. Carvedilol therapy was to be discontinued at discharge and replaced with an alternate antihypertensive regimen.
Discussion: This patient presents with circulatory shock due to AV blockade from beta-blocker therapy likely incited by an acute kidney injury with urinary tract infection. The recently recognized clinical entity referred to as Bradycardia-Renal Failure-AV Nodal Blockade-Shock-Hyperkalemia (BRASH) syndrome accurately characterizes this presentation. The pathophysiology of BRASH syndrome entails the synergistic effects of hyperkalemia and renally-excreted AV-nodal blocking medications in patients with a renal insult culminating in circulatory shock. The epidemiology and mortality of BRASH is not well-characterized due to its recent recognition; nonetheless there appears to be an increased prevalence in geriatric patients with cardiac and renal disease as well as those on multiple AV nodal blocking agents.
Conclusions: The diagnosis of BRASH is made clinically and requires a high index of suspicion. Management of this condition involves prompt recognition and discontinuation of AV-nodal blockade, administration of calcium to stabilize the cardiac membrane, management of hyperkalemia with insulin, augmentation of cardiac output and vascular tone with inotropic and vasopressor therapy, and treatment of underlying acute kidney injury; definitive management of refractory renal dysfunction and hyperkalemia is emergent hemodialysis. Early recognition of this syndrome may prevent permanent pacemaker placement.