Case Presentation: Fibrillary glomerulonephritis and immunotactoid glomerulopathy are rare renal disorders, being present in 0.5 to 1.4 percent of kidney biopsies. Although they are distinct glomerulopathies, they are both nonamyloid fibrillary glomerular diseases and as such, they are Congo red negative on immunohistochemistry.
Discussion: Patient is a 75 years old male with PMH of HTN, diabetes type II, diabetic nephropathy, CKD stage III, hypothyroidism, and CHF who was initially admitted to the hospital for shortness of breath and increased bilateral leg edema. Labs showed evidence of AKI with a creatinine of 4.30 mg/dL and baseline of 2.5 mg/dL. Associated GFR was 12.57 ml/min/ 1.73m2. Cardiac workup included echocardiogram which showed left ventricular ejection fraction of 42% and nuclear cardiac stress test which did not show significant perfusion abnormalities. V/Q scan showed low probability for pulmonary embolus. Renal workup was performed on an outpatient basis with urinalysis demonstrating 2+ blood (RBC 47 per HPF), protein 1+ and urine random protein to creatinine ratio of 5654 mg/g (range 22-128). Although the patient had baseline risk factors of hypertension and diabetes, additional studies were pursued to investigate the acute renal failure (ARF).
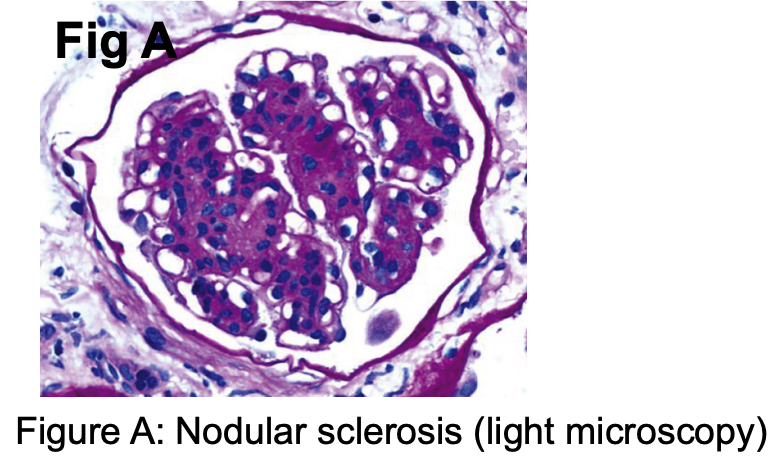
Conclusions: Serology came back as C-ANCA positive (titer 1:1280), however since ANCA titer does not necessarily correlate with disease activity, paraproteinemia was also considered in the differential diagnosis. Although serum protein electrophoresis was normal, urine protein electrophoresis was positive for a monoclonal spike. Kidney biopsy was then obtained and the pathology showed immunotactoid glomerulopathy with lambda restriction, consistent with a monoclonal gammopathy of renal significance. Histologically, the key diagnostic features include mesangial proliferation, clonal IgG and light chain restriction, and microtubules in parallel arrays in the mesangium with diameter >30 nm (Figs A, B). Since immunotactoid glomerulopathy involves circulating monoclonal paraproteinemia, a lympho- plasmacytic malignancy is often present. Hence, the patient is currently referred to a hematology oncologist for bone marrow biopsy for evaluation of possible malignancy such as multiple myeloma. If the hematologic workup is inconclusive, then fludarabine or a combination of high-dose methylprednisolone and rituximab followed by alemtuzumab has been shown to reduce proteinuria and improve renal function.