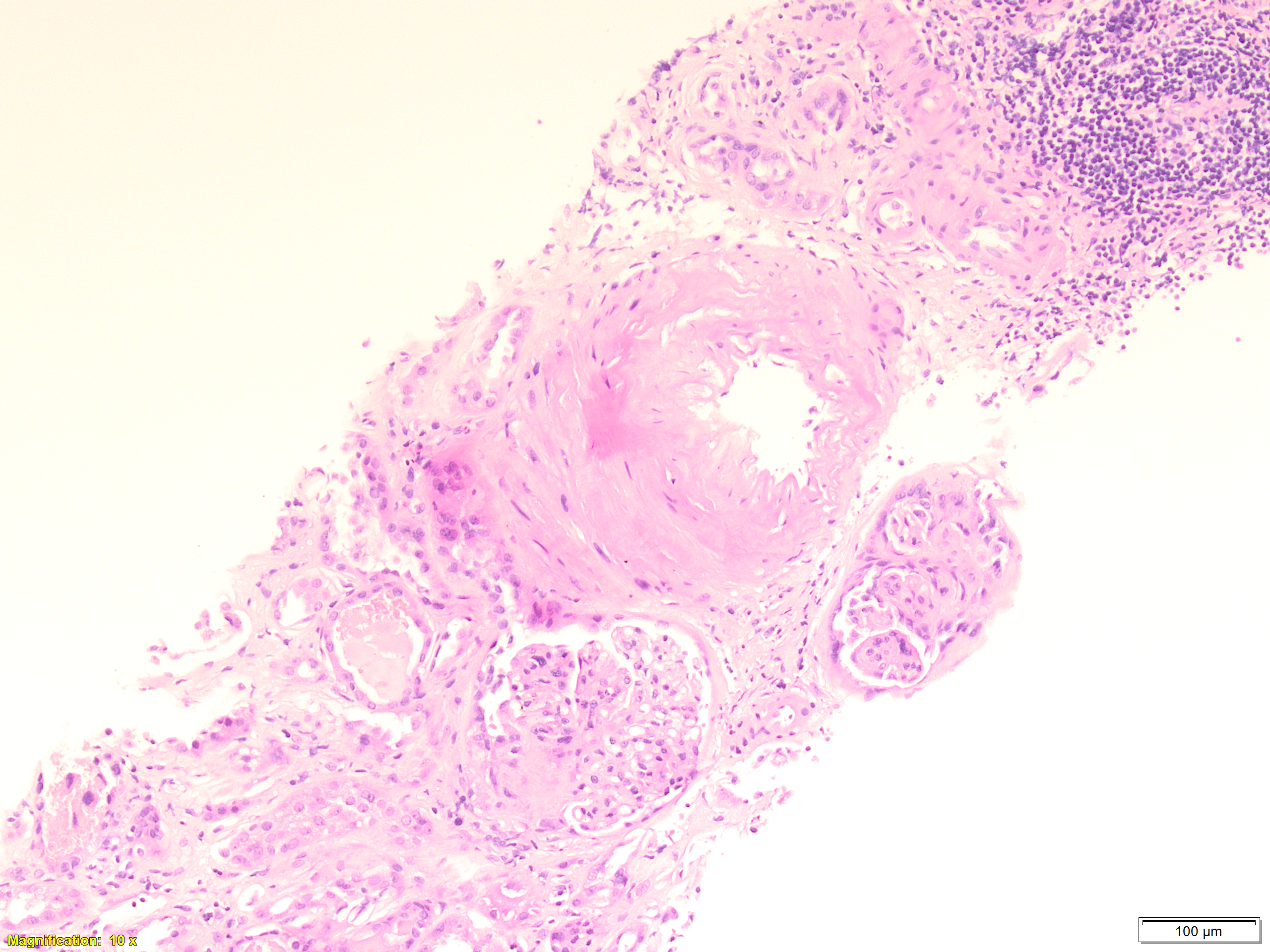
Case Presentation: A 79-year-old woman with a past medical history of uncontrolled hypertension, migraine, and chronic kidney disease stage 3 presented with one week of poor oral intake, nausea, vomiting, vague abdominal pain, and chronic nonproductive cough. Physical exam revealed poor skin turgor, and lungs with crackles bilaterally. Laboratory studies showed Creatinine of 5.31 mg/dl from a baseline of 2.6 mg/dl, urinalysis was significant for 3+ protein and blood. Renal imaging showed no hydronephrosis. Patient was started on fluid resuscitation due to concern of pre-renal acute kidney injury (AKI). Despite fluid resuscitation, her creatinine continued to be elevated. Additional studies including urine and serum protein electrophoresis, immunofixation (IFE), hepatitis, and ANA were normal. However, antineutrophil cytoplasmic antibodies (PR3-ANCA) and perinuclear anti-neutrophil cytoplasmic antibodies (MPO-ANCA) titers were both elevated. Renal biopsy was performed and revealed drug induced pauci-immune crescentic glomerulonephritis (Image 1). Computed Tomography (CT) of the chest as part of chronic cough work up showed mild bilateral ground glass opacity (GGO) (Image 2). Transthoracic echocardiogram (TTE) was performed and showed pulmonary hypertension and Pulmonary arterial systolic pressure (PASP) of 52 mmHg. Detailed medication history revealed that the patient had been on hydralazine 100mg twice daily for 7 years for uncontrolled hypertension and was stopped one month before presentation. Hence, diagnosis of hydralazine induced ANCA associated vasculitis was made. Patient was started on Rituximab and pulse dose of steroid. Her kidney function significantly improved thereafter and was discharged in a stable condition. Upon follow up few months later, her creatinine returned to baseline and all of her symptoms resolved. Repeat imagining showed resolution of bilateral GGO and repeat TTE showed reduction of PASP to 31.
Discussion: Hydralazine induced ANCA associated vasculitis (AAV) is, although rare, a widely known side effect with an incidence of 5.4%–10.4%, particularly in patients who are slow acetylators (1). The ANCA complex activates inflammatory pathways leading to inflammation of the small vessels and, as result, damage to highly microvascular organs including the kidneys and lungs. The renal clinical manifestation AAV can vary from acute kidney injury to rapidly progressive glomerulonephritis and end stage renal disease (ESRD) from irreversible kidney injury (glomerulosclerosis and interstitial fibrosis) (2). Its pulmonary presentation can also vary from interstitial lung disease to pulmonary alveolar hemorrhage, coining AAV disease as drug induced pulmonary renal syndrome. Our case demonstrates a unique presentation of pulmonary renal syndrome in which the presentation was late and 1 month after the discontinuation of the culprit medication and not as reported before (3) which usually presents while on treatment.
Conclusions: Hydralazine is a commonly used anti-hypertensive and heart failure medication. It is well known to be associated with several autoimmune diseases including drug induced lupus and ANCA associated vasculitis (AAV) which can involve the kidney and less commonly other organs. In this case we describe an acute kidney injury, which after thorough investigation evolved into Hydralazine induced pulmonary-renal syndrome. A condition that is associated with high risk of mortality, but can be prevented by early awareness and appropriate treatment.